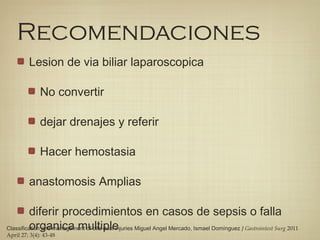
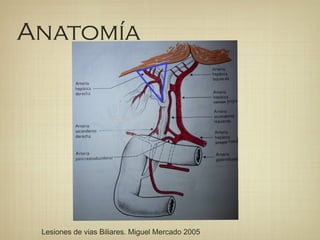
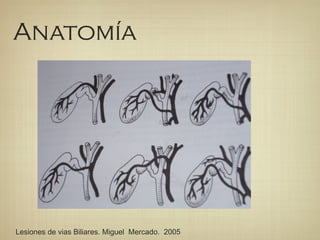
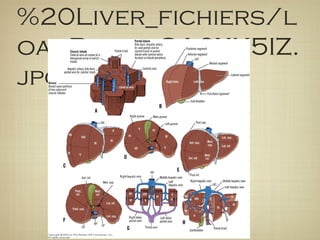
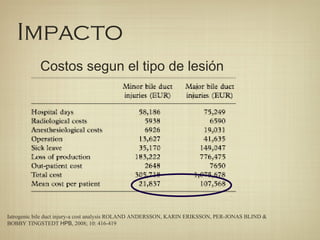
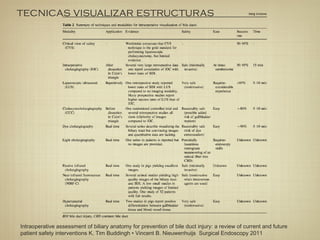
This document provides information on the diagnosis and management of biliary tract injuries. It begins with an overview of biliary anatomy and classifications of injuries. Key points include:
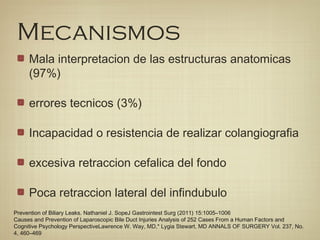
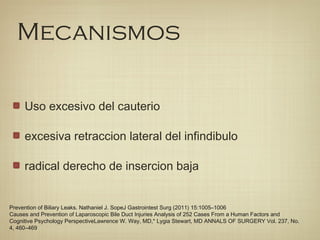
- Biliary injuries can occur during cholecystectomy and liver transplantation. Common mechanisms involve misidentifying structures and thermal or mechanical damage.
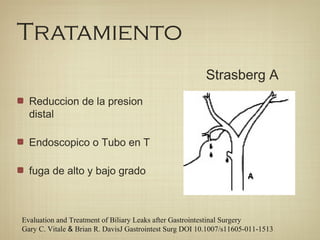
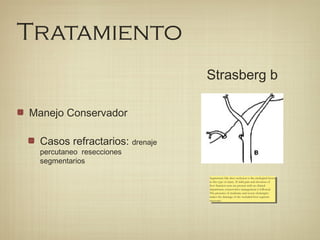
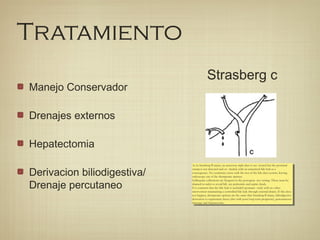
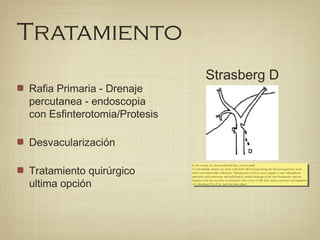
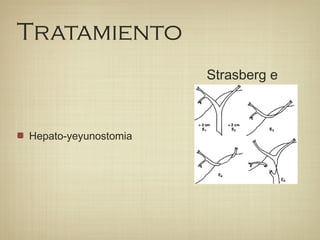
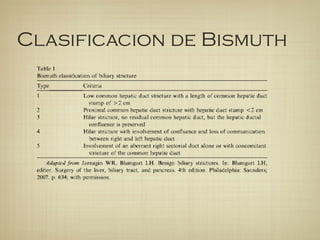
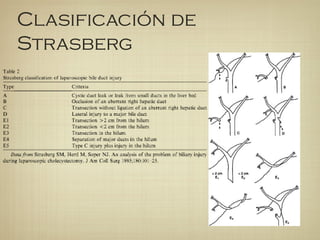
- Injuries are classified using systems like Bismuth and Strasberg to determine severity and guide treatment.
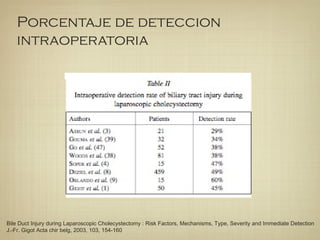
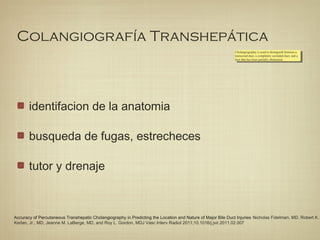
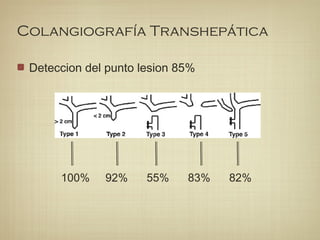
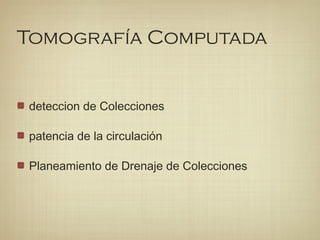
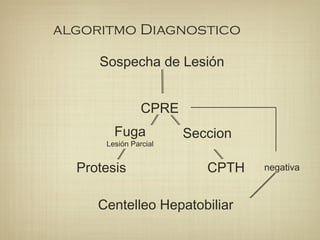
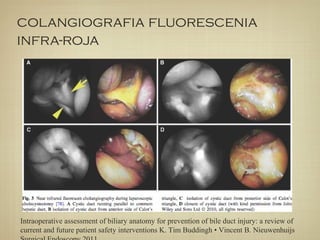
- Diagnosis may involve intraoperative identification of bile leaks or postoperative imaging like MRCP or ERCP. Transhepatic cholangiography provides the best view of anatomy.
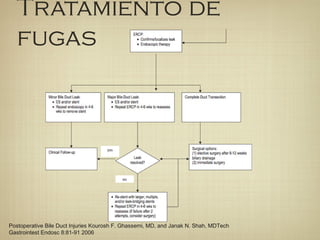
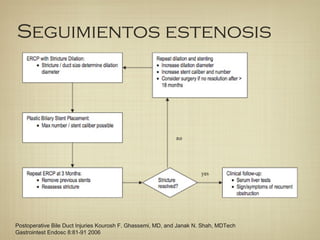
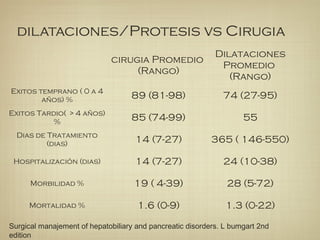
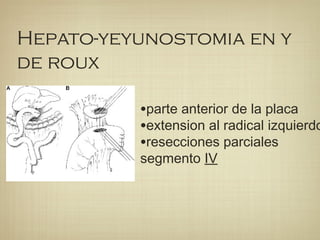
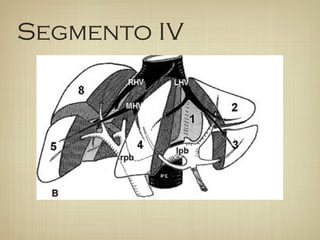
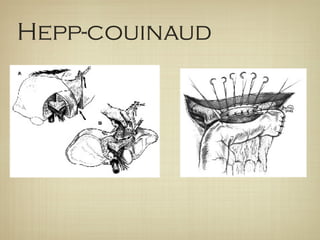
- Treatment depends on injury type but may include drainage, stenting, resection, or bilioenter
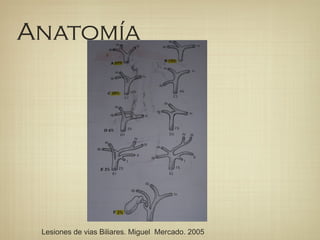
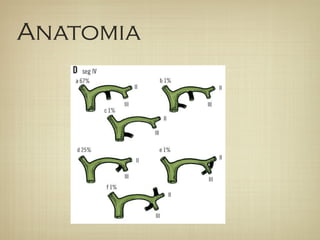

![Clasificacion de Stewart-way
Class I refers to the incomplete sectionof
bile duct with no loss of tissue. It has a
prevalence rate of 7%. The first mechanism of injury
is a misleading recognition of the common hepatic
duct with the cystic duct but is rectified and results in
only a small loss of tissue with no complete section of
the bile duct. The second mecha- nism refers to the
lateral injury of the common hepatic duct which
results from the cystic duct opening extension during
cholangiography. The former represents 72% and the
latter 28% of class I cases.
Class I refers to the incomplete sectionof
bile duct with no loss of tissue. It has a
prevalence rate of 7%. The first mechanism of injury
is a misleading recognition of the common hepatic
duct with the cystic duct but is rectified and results in
only a small loss of tissue with no complete section of
the bile duct. The second mecha- nism refers to the
lateral injury of the common hepatic duct which
results from the cystic duct opening extension during
cholangiography. The former represents 72% and the
latter 28% of class I cases.
Class II is a lateral injury of the common hepatic duct
that leads to stenosis or bile leak. It is the
consequence of thermal damage and clamping the
duct with surgical
staples. It has a prevalence of 2% with a concomitant
he- patic artery injury in 18% of cases. T-tube related
injuries are included within this class.
Class II is a lateral injury of the common hepatic duct
that leads to stenosis or bile leak. It is the
consequence of thermal damage and clamping the
duct with surgical
staples. It has a prevalence of 2% with a concomitant
he- patic artery injury in 18% of cases. T-tube related
injuries are included within this class.
Class III is the most common (61% of cases) and rep-
resents the complete section of the common hepatic
duct. It is subdivided in to type IIIa, remnant
common hepatic duct; type IIIb, section at the
confluence; type IIIc, loss of confluence; and type
IIId, injuries higher than confluence with section of
secondary bile ducts. It occurs when the common
hepatic duct is confounded with the cystic duct,
leading to a complete section of the common hepatic
duct when resecting the gallbladder. A concomitant
injury of right hepatic artery occurs in 27% of cases
Class III is the most common (61% of cases) and rep-
resents the complete section of the common hepatic
duct. It is subdivided in to type IIIa, remnant
common hepatic duct; type IIIb, section at the
confluence; type IIIc, loss of confluence; and type
IIId, injuries higher than confluence with section of
secondary bile ducts. It occurs when the common
hepatic duct is confounded with the cystic duct,
leading to a complete section of the common hepatic
duct when resecting the gallbladder. A concomitant
injury of right hepatic artery occurs in 27% of cases
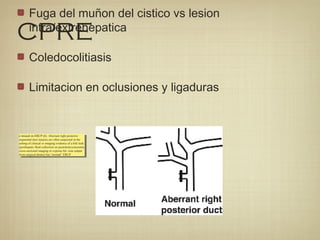
Class IV describes the right (68%) and accessory right
(28%) hepatic duct injuries with concomitant injury of
the right hepatic artery (60%). Occasionally it includes
the common hepatic duct injury at the confluence
(4%) besides the accessory right hepatic duct lesion.
Class IV has a prevalence of 10%[11,12].
Class IV describes the right (68%) and accessory right
(28%) hepatic duct injuries with concomitant injury of
the right hepatic artery (60%). Occasionally it includes
the common hepatic duct injury at the confluence
(4%) besides the accessory right hepatic duct lesion.
Class IV has a prevalence of 10%[11,12].](https://image.slidesharecdn.com/lesionbililarfinalle-140708231806-phpapp02/85/LESION-DE-VIA-BILIAR-28-320.jpg)