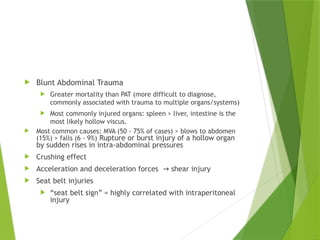
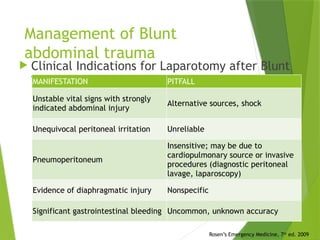
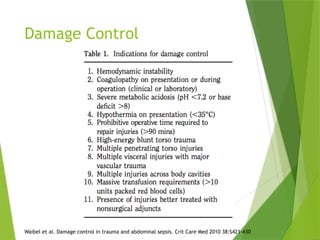
The document discusses the management and classification of abdominal trauma, including penetrating and blunt trauma, their mechanisms, and common injuries. It outlines initial assessments, diagnostic studies, and treatment protocols such as laparotomy, damage control principles, and the role of imaging techniques. Additionally, it emphasizes the importance of timely interventions based on clinical indications, including the evaluation of patients' hemodynamic stability.