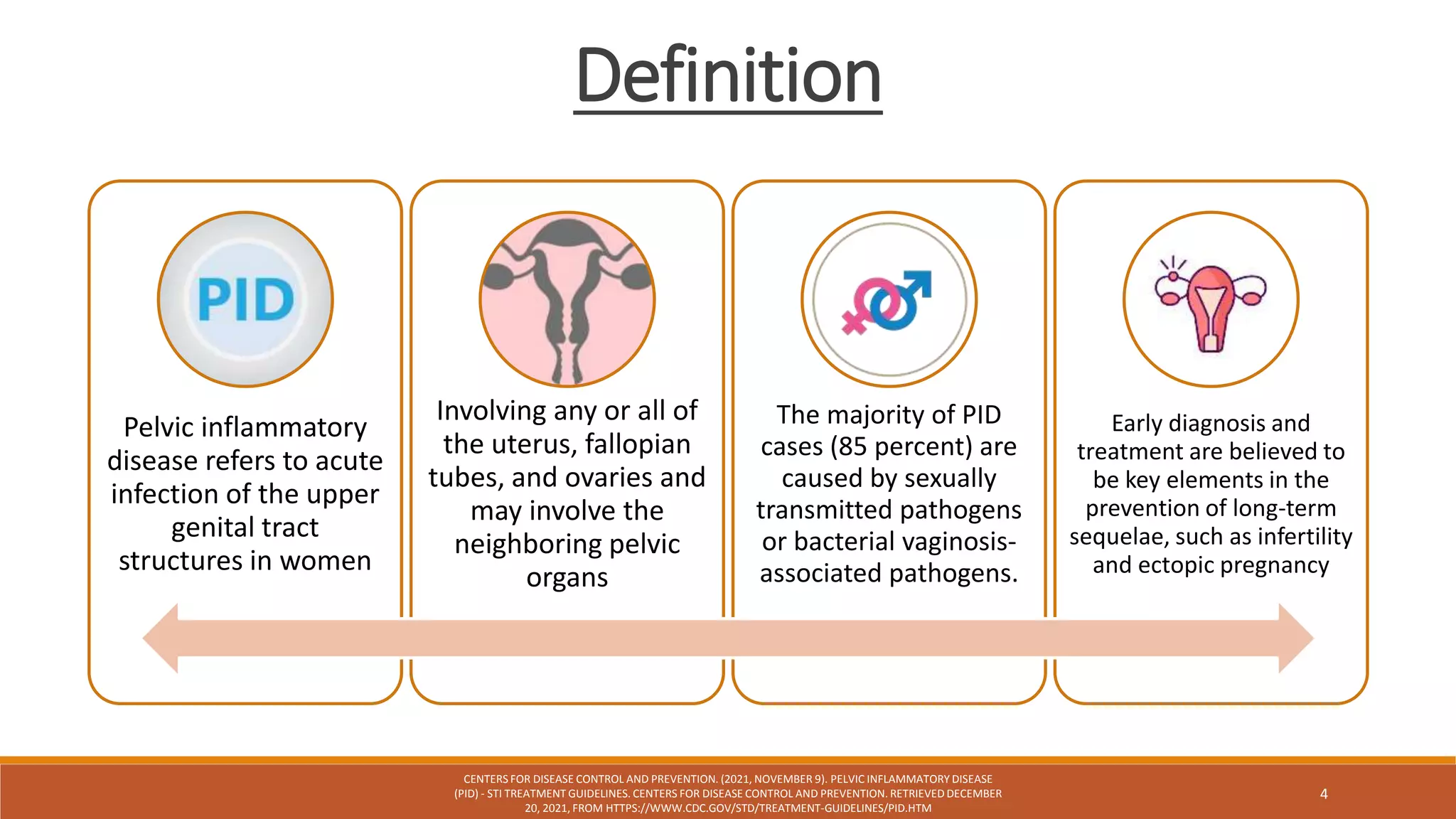
This document outlines a randomized controlled trial comparing ceftriaxone and doxycycline, with or without metronidazole, for treating acute pelvic inflammatory disease (PID) in women. The study investigates treatment effectiveness and evaluates clinical outcomes of both regimens, reporting no significant advantages of adding metronidazole. Overall, the trial highlights the need for clear treatment guidelines amid existing uncertainties about the benefits of broader anaerobic coverage.