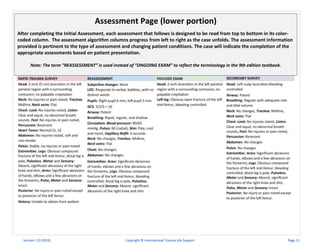
The document outlines the International Trauma Life Support (ITLS) case-based learning scenarios aimed at enhancing trauma care for emergency providers. It details the objectives, attributes, challenges of case-based learning, and provides guidelines for using ITLS scenarios effectively, including assessment and evaluation rubrics. Additionally, it emphasizes the importance of experiential learning and instructor-guided discussions to facilitate learner engagement and skill mastery.











![Page 1 of 4 (Abdominal Trauma 1P-1)
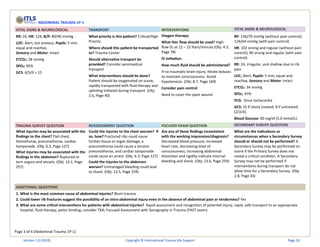
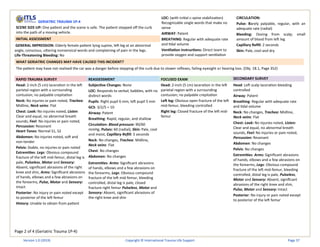
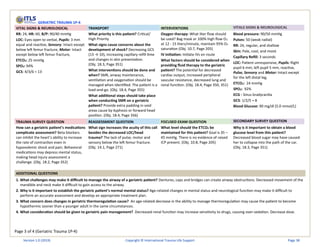
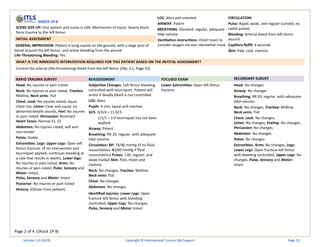
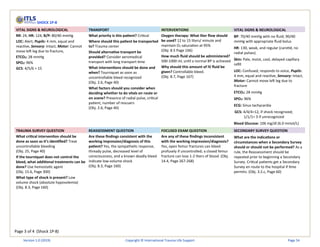
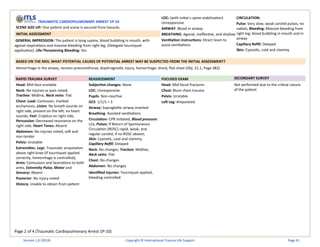
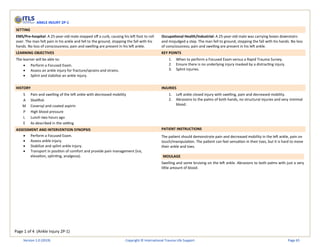
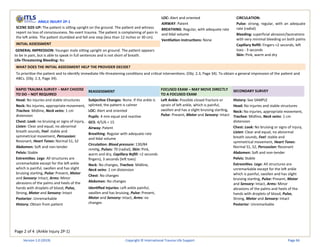
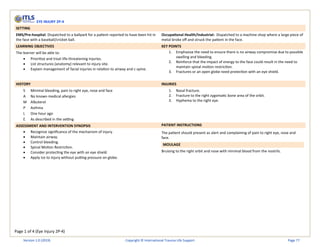
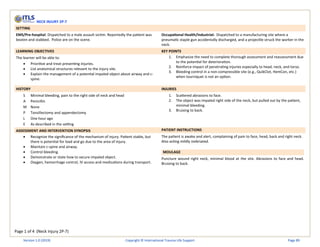
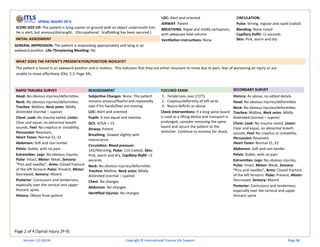
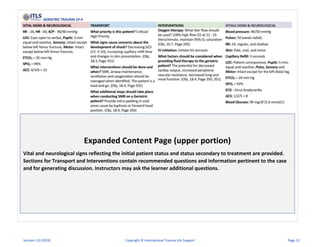
ABDOMINAL TRAUMA 1P-1
SETTING
EMS/Pre-hospital: An ambulance has been dispatched to a local sports stadium for an
injured soccer/football player who collided with a metal bench on the sidelines.
Occupational Health/Industrial: An ambulance has been dispatched to the warehouse
for an injured employee who was struck by a forklift.
LEARNING OBJECTIVES KEY POINTS
The learner will be able to:
• Identify a critical blunt abdominal injury and identify associated
complications.
• Assess and manage a critical trauma patient with a blunt abdominal injury.
• Describe possible intra-abdominal injuries based on findings of history,
physical examination, and mechanism of injury.
1. Blunt trauma is the most common cause of abdominal injuries.
2. Blunt trauma may be from direct compression of the abdomen against a fixed
object resulting in tears or subcapsular hematomas involving solid intra-
abdominal organs (liver/spleen).
3. Injuries may arise from deceleration forces, with tearing of organs and their
blood vessels at fixed areas within the abdominal region.
4. Lower rib fractures suggest the possibility of an intra-abdominal injury even
in the absence of abdominal pain or tenderness.
5. Be prepared to treat hypovolemic shock from occult intra-abdominal
bleeding.
6. Blunt abdominal trauma with pain or tenderness may indicate serious
abdominal trauma and the potential for quick development of shock even if
initial vital signs are normal.
HISTORY INJURIES
S Left-sided lower rib pain and wrist pain
A None
M Albuterol, Solu-Medrol, naproxen and ibuprofen
P Asthma
L Sports drink 30 minutes
E As described in the setting
1. Intra-abdominal bleeding
2. Left lower rib fractures
3. Shock
4. Open left distal radial fracture
ASSESSMENT AND INTERVENTION SYNOPSIS PATIENT INSTRUCTIONS
• Recognize significant Mechanism of Injury and load and go
• Recognize difficulty breathing and delegate high-flow O2
• Recognize significance of injuries to chest, abdomen and the potential for rapid
deterioration
• Initiate fluid therapy during transport titrated to maintain level of
consciousness, and avoid hypotension
• Recognize significance of evolving changes in abdominal presentation
• Obtain a blood glucose level
• Consider aeromedical transport
• Consider pain control
• Splint wrist fracture if time allows
Patient should be alert, but anxious and complaining of left-sided rib pain, left wrist
pain and left shoulder (referred pain). Complain of pain on left side of abdomen only
when upper left quadrant is palpated. Speak in short sentences (2-3 words) due to rib
pain. Simulate shallow and rapid respirations if able to do so safely. No head, neck or
back pain and no loss of consciousness.
MOULAGE
Open left wrist fracture with minor distracting bleeding. (If open fracture is not
possible, show bruising over the left wrist [closed fracture]). Bruising to lower left ribs
on the mid-axillary line. Simulate shock with pale and moist skin.
Version 1.0 (2019) Copyright © International Trauma Life Support Page 24](https://image.slidesharecdn.com/itls-case-based-learning-scenarios-version-1-240612130354-950cdb04/85/ITLS-Case-Based-Learning-Scenarios-Version-1-0-2019-pdf-24-320.jpg)