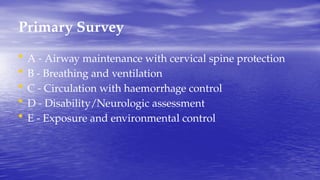
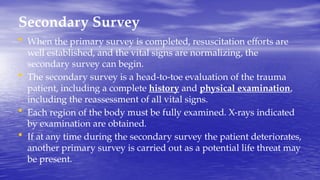
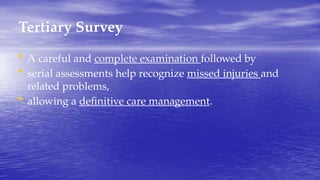
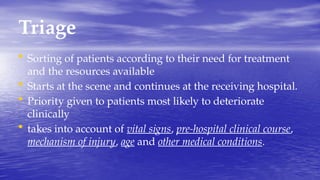
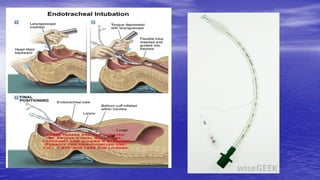
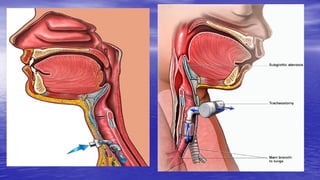
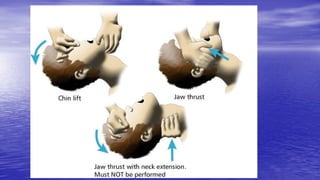
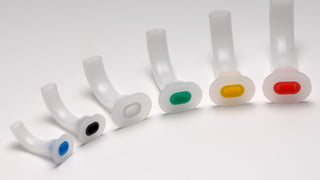
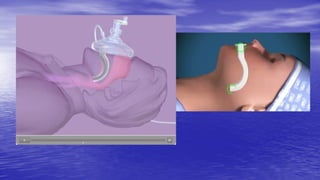
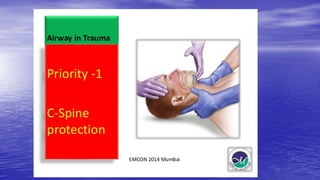
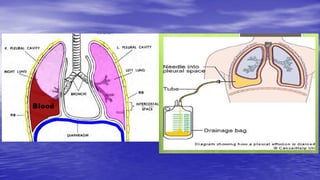
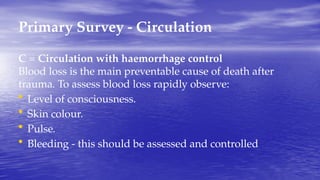
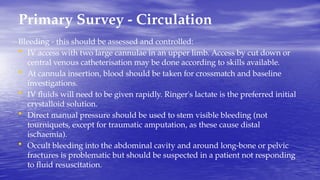
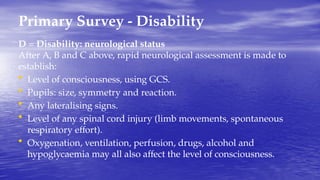
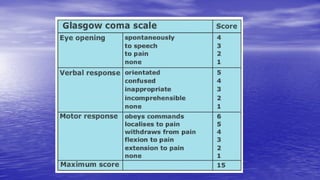
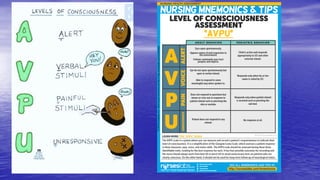
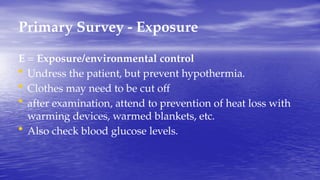
The document outlines the field of traumatology, which focuses on injuries and wounds caused by accidents or violence, including both medical and psychological aspects. It discusses the Advanced Trauma Life Support (ATLS) program, emphasizing the importance of systematic patient assessment and management through primary, secondary, and tertiary surveys. Key principles include airway management, controlling hemorrhage, and conducting thorough evaluations to ensure effective treatment of trauma patients.