This document provides an overview of pharmacy residency programs, including:
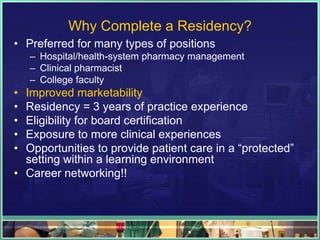
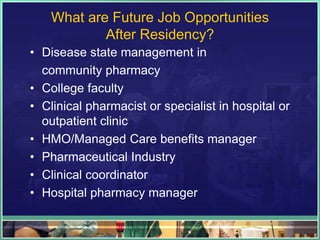
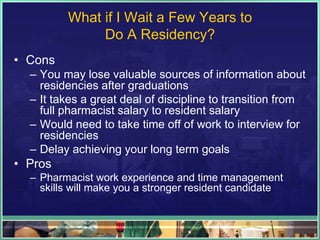
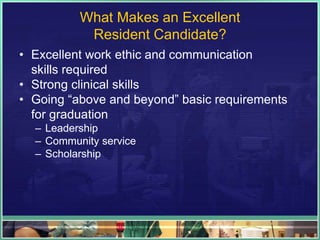
- Residency programs are becoming increasingly important for pharmacists to gain direct patient care experience and be eligible for board certification.
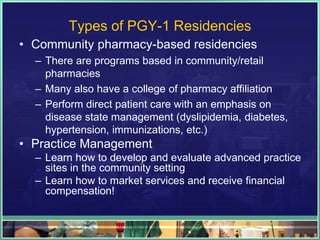
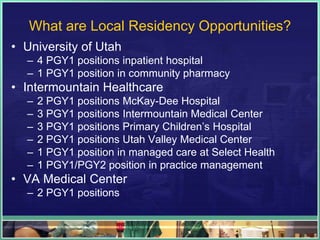
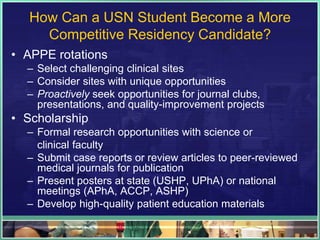
- Residencies allow pharmacists to build clinical skills through postgraduate training opportunities in various settings like hospitals, clinics, and retail pharmacies.
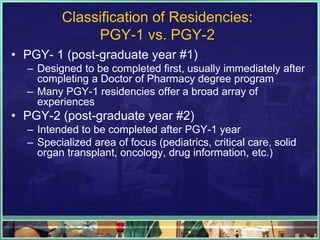
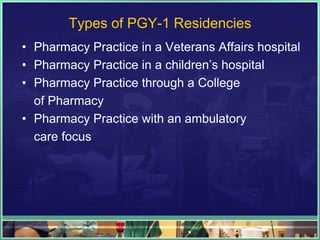
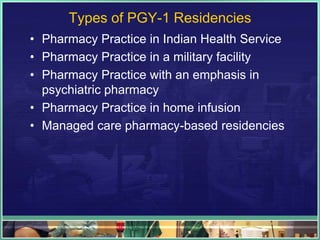
- The most common types of residencies are PGY-1 programs which provide a broad range of experiences, and PGY-2 programs which offer more specialized training.
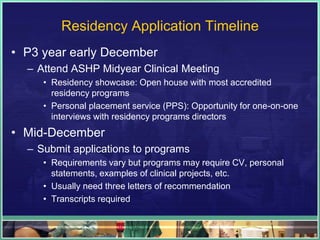
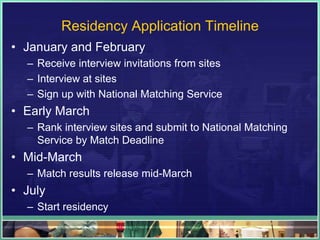
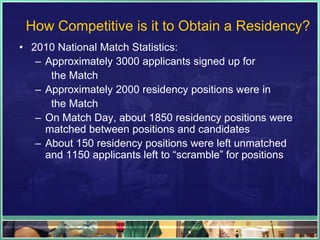
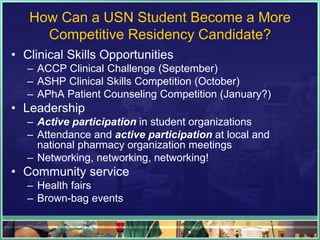
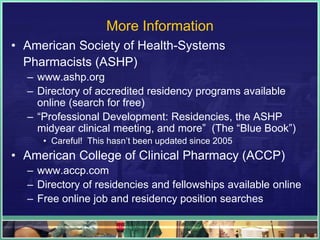
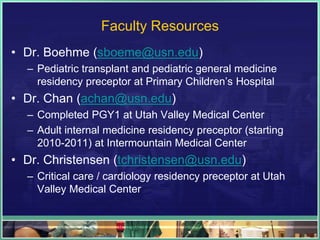
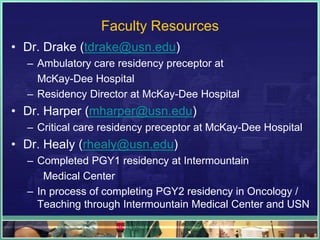
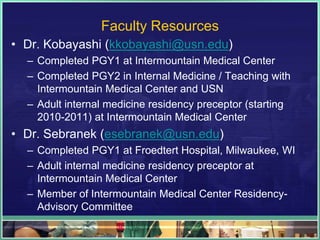
- Obtaining a competitive residency position requires strong clinical skills, leadership experience, and networking at events like the ASHP Midyear meeting. Faculty at the University of Utah can provide guidance