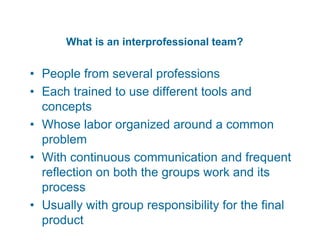
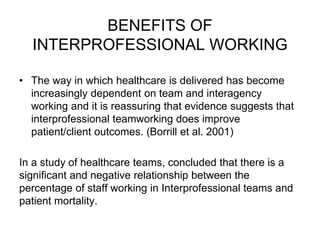
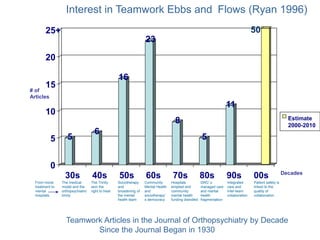
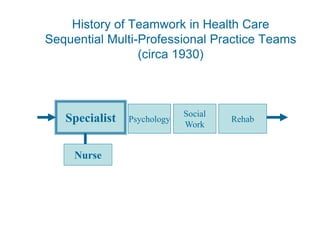
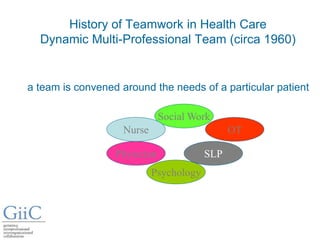
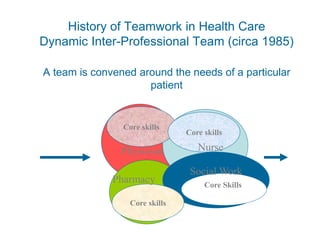
An interprofessional team consists of professionals from different fields who work together to address a common problem. The benefits of interprofessional teams include improved patient outcomes. Studies have found lower patient mortality rates when more staff work on interprofessional teams. As populations age, interprofessional collaboration will become increasingly important to address older patients' multiple and long-term needs, which often require input from different healthcare professionals and agencies. Interprofessional practice is also relevant outside of healthcare, as professionals from various public, private, and nonprofit sectors may collaborate to help individuals. While interest in teamwork has fluctuated over time, patient safety and quality improvement initiatives are currently driving greater focus on interprofessional care.