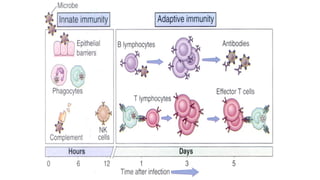
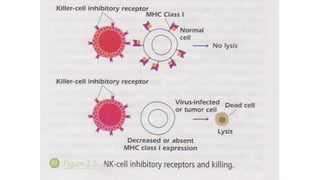
The document outlines the key components and functions of the innate immune system, which serves as the first line of defense against invading microorganisms. It distinguishes between the innate and adaptive immune systems, detailing various defense mechanisms such as anatomical, physiological, and phagocytic barriers. Additionally, it describes the roles of specific immune cells, including natural killer cells and macrophages, in protecting the body from infections and restoring immune homeostasis during inflammation.