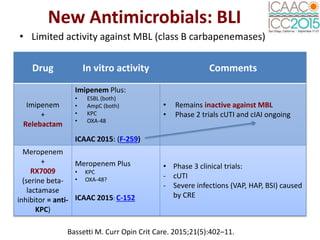
This document provides an outline of José Ramón Paño-Pardo's track at the ICAAC 2015 conference. The conference focused on antimicrobial agents and chemotherapy. Key topics included antimicrobial stewardship, bloodstream infections, new antimicrobials, and clinical infectious disease syndromes. Sessions covered emerging resistance issues like carbapenemase-producing Enterobacteriaceae and rapid diagnostics for sepsis.