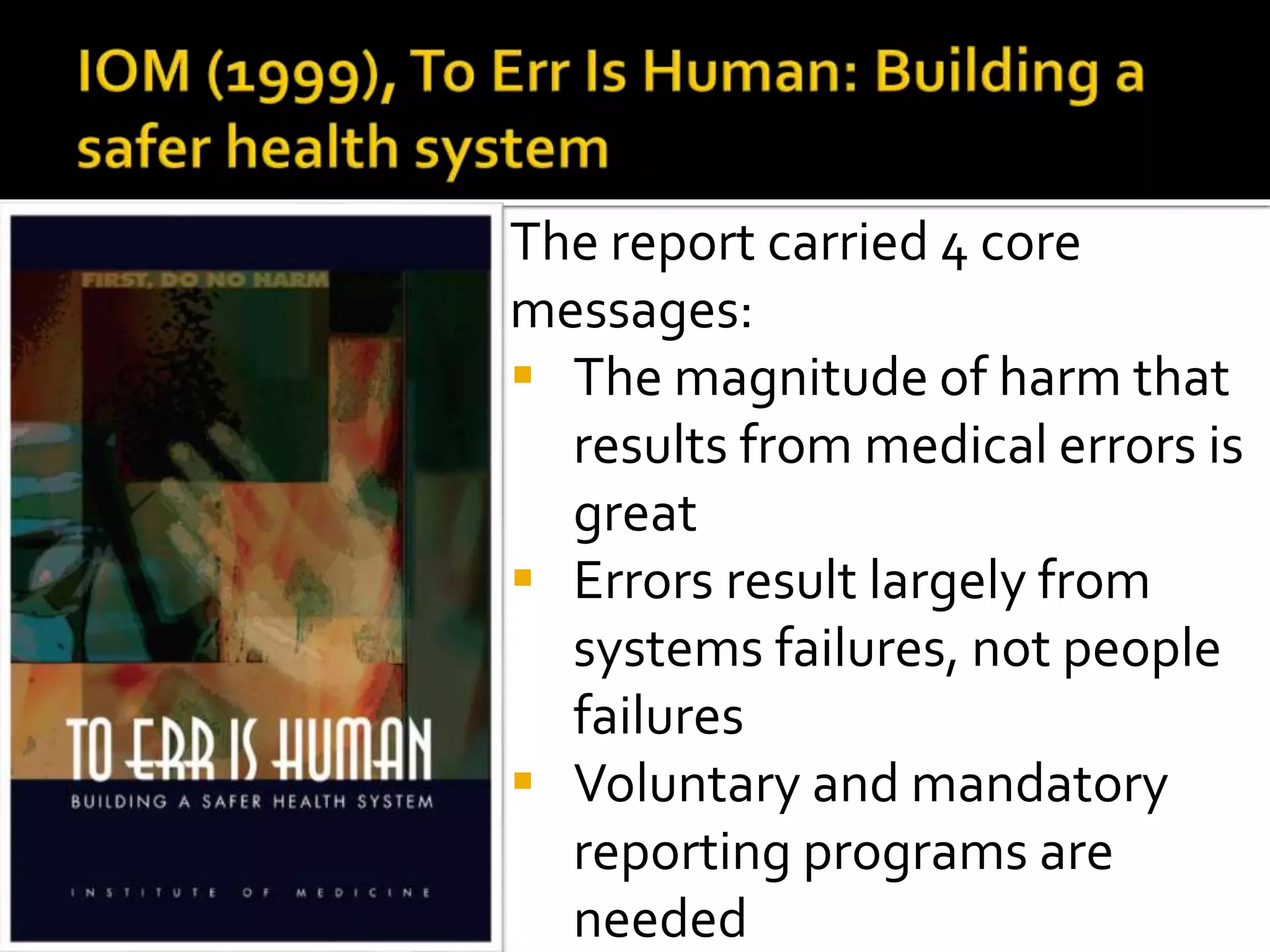
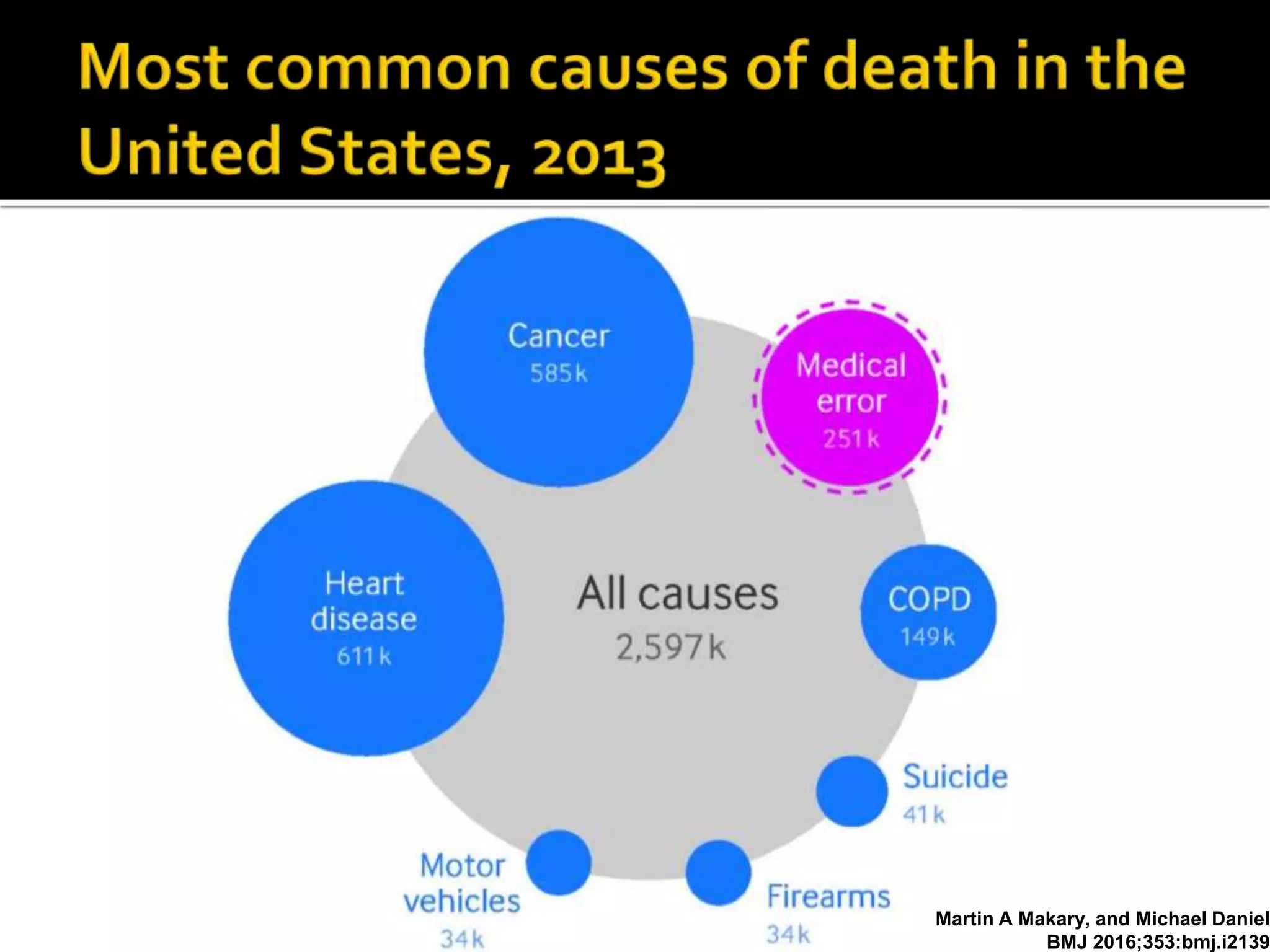
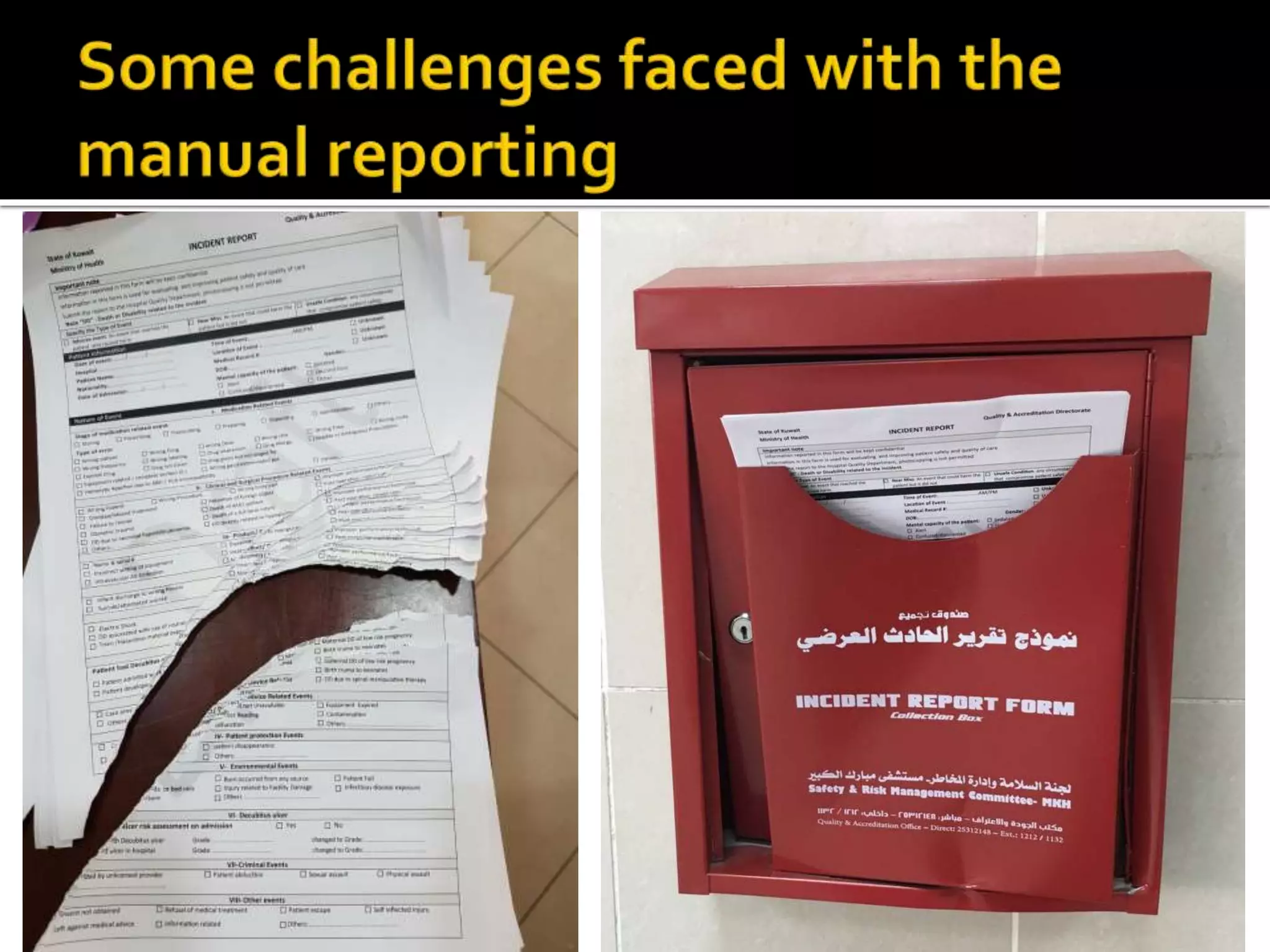
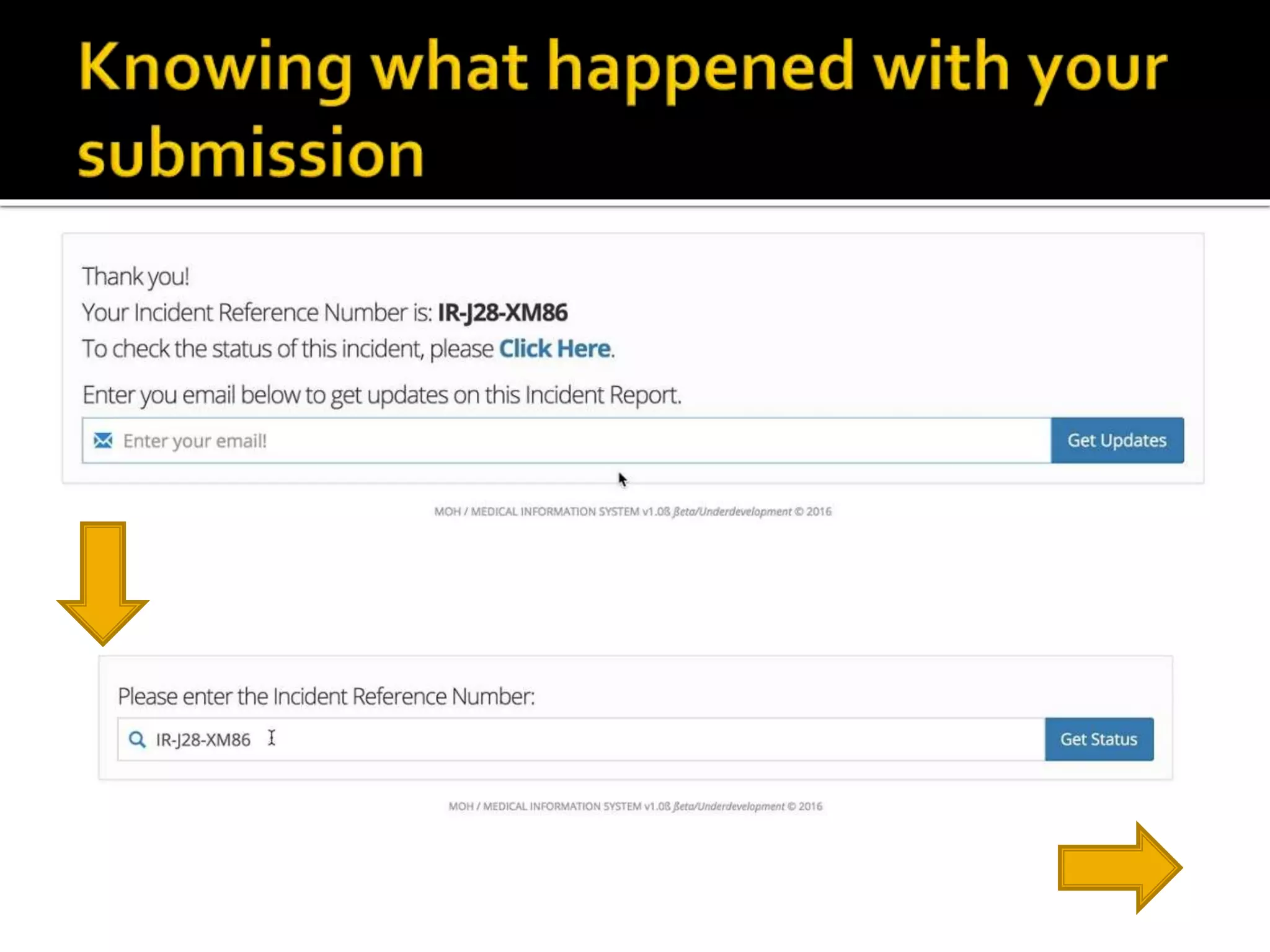
This document discusses patient safety incident reporting and identifies barriers to reporting. It notes that reporting is important for detecting safety issues but is often limited by lack of feedback and fears of punishment. A study found the major barriers to reporting were lack of feedback, limited reporting methods, and fears of consequences. The document proposes a mobile app to make incident reporting easier, anonymous, and provide real-time feedback to encourage reporting. The app would use data to identify safety issues and measure harm reduction efforts.













![1. AHRQ. Voluntary Patient Safety Event Reporting (Incident Reporting) |
AHRQ Patient Safety Network [Internet]. 2014 [cited 2016 Apr 10].
Available from:
https://psnet.ahrq.gov/primers/primer/13/voluntarypatientsafetyeventr
eportingincidentreporting
2. Lawton R, Parker D. Barriers to incident reporting in a healthcare
system. Qual Saf Health Care. 2002;11(1):15–8.
3. Noble DJ, Pronovost PJ. Underreporting of patient safety incidents
reduces health care’s ability to quantify and accurately measure harm
reduction. J Patient Saf. 2010 Dec;6(4):247–50.
4. Mahajan RP. Critical incident reporting and learning. Br J Anaesth.
2010;105(1):69–75.](https://image.slidesharecdn.com/ireport-160524194822/75/I-report-23-2048.jpg)