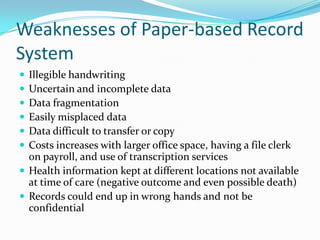
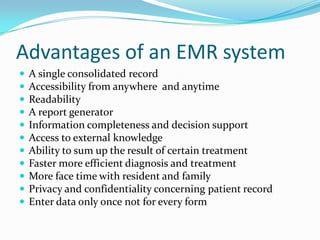
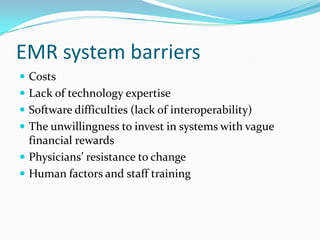
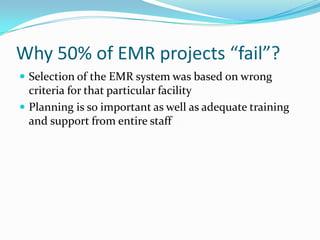
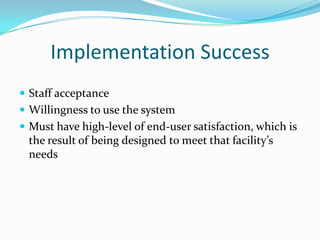
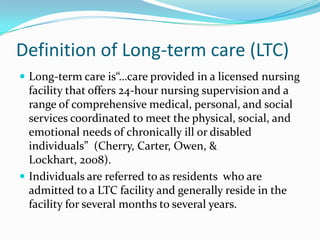
This case study investigates the implementation of a hybrid electronic medical record (EMR) system in a long-term care (LTC) facility, highlighting the weaknesses of paper-based records and advantages of EMR. It discusses barriers to adoption, reasons for project failures, and emphasizes the importance of staff acceptance and training for successful implementation. The study concludes that EMR systems can significantly enhance care quality and operational efficiency in LTC settings.