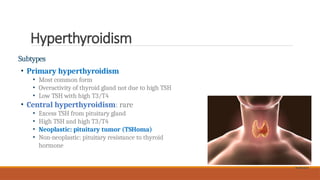
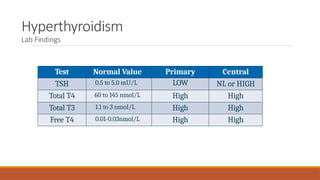
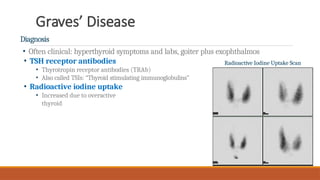
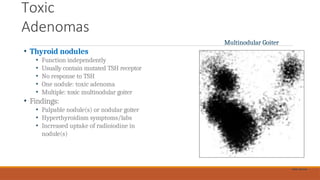
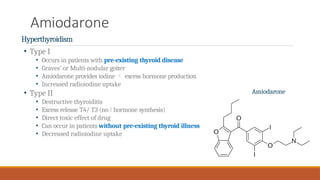
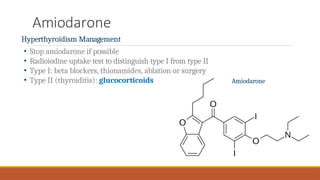
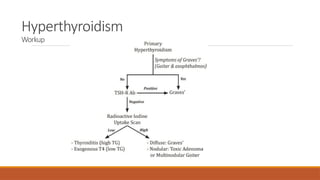
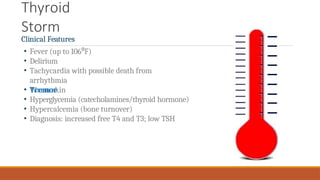
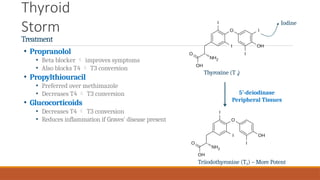
The document discusses hyperthyroidism, characterized by excessive thyroid hormone production leading to symptoms such as weight loss, heat intolerance, and tachycardia. It covers various subtypes, including primary and central hyperthyroidism, causes like Graves' disease and toxic adenomas, and treatment options including beta blockers and radioiodine ablation. Additionally, it highlights the critical condition of thyroid storm and its management.