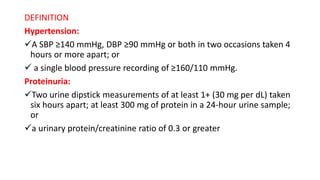
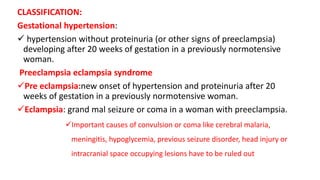
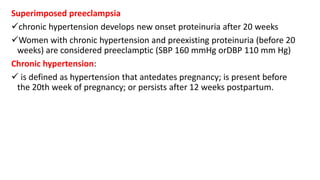
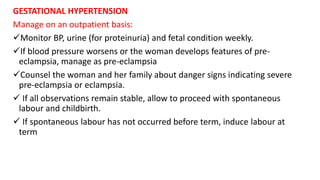
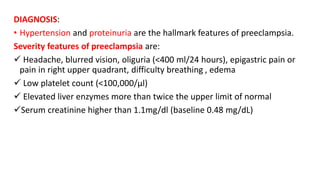
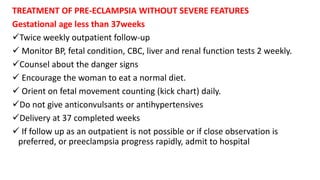
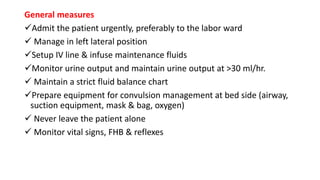
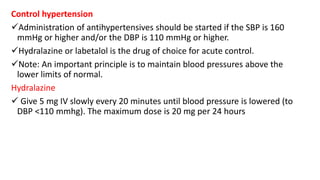
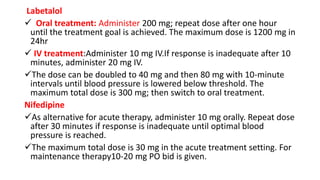
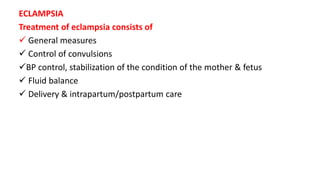
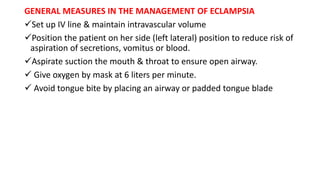
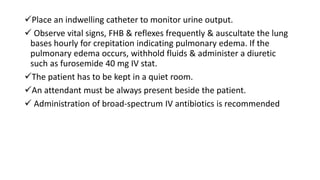
The document defines and classifies hypertensive disorders in pregnancy including gestational hypertension, preeclampsia, eclampsia, and chronic hypertension. It describes the risk factors, diagnosis, and management of these conditions. Key points include:
- Preeclampsia is defined as new onset hypertension and proteinuria after 20 weeks of gestation.
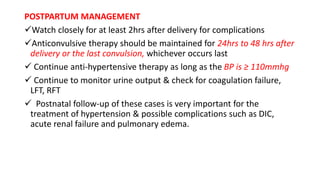
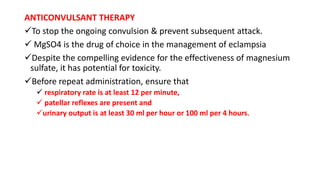
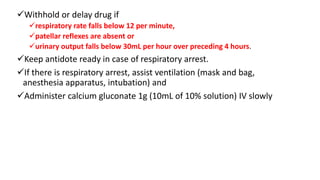
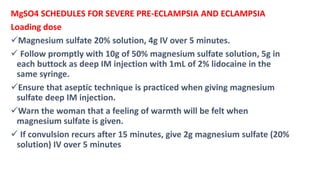
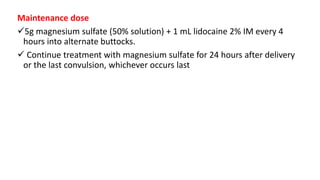
- Magnesium sulfate is the primary treatment for preventing seizures in preeclampsia and eclampsia.
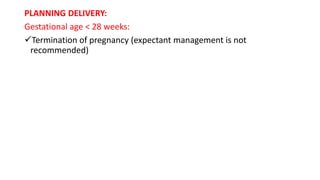
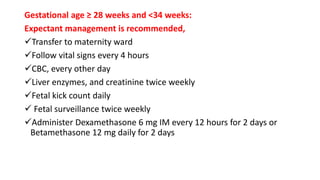
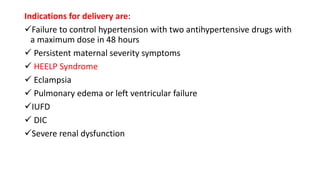
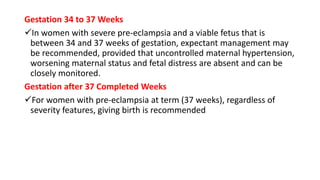
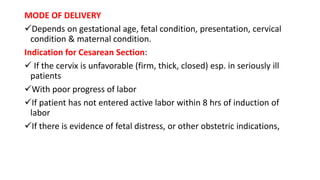
- Delivery is usually indicated for preeclampsia between 28-37 weeks of gestation or by term for control of maternal symptoms and blood pressure.