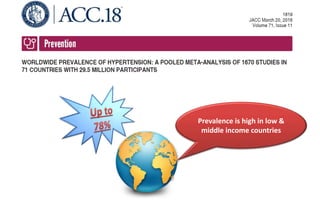
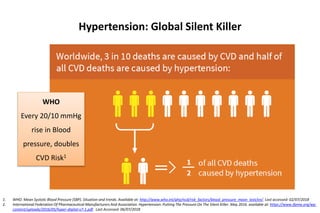
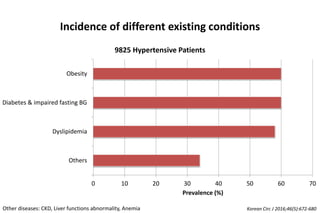
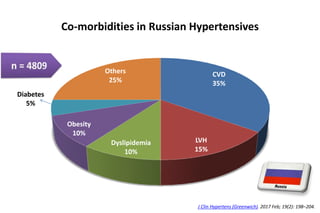
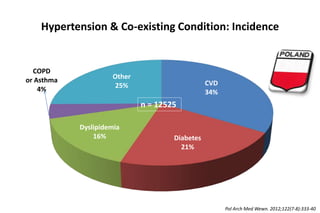
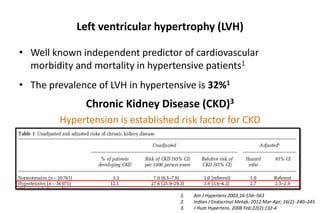
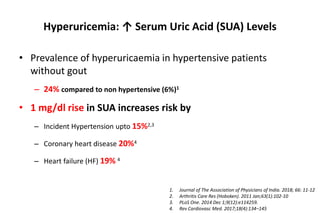
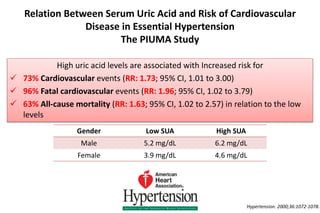
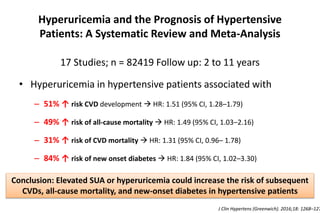
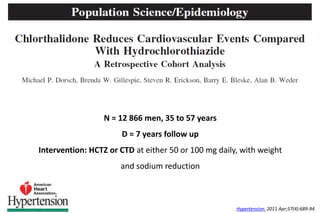
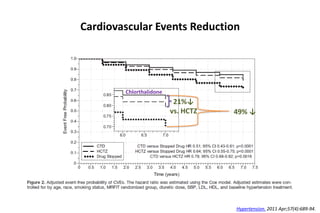
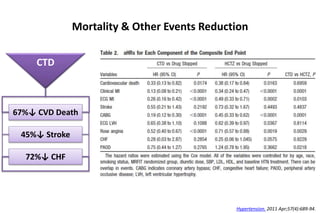
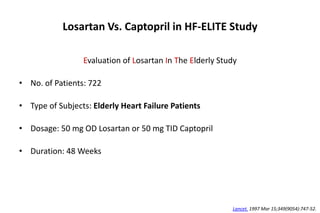
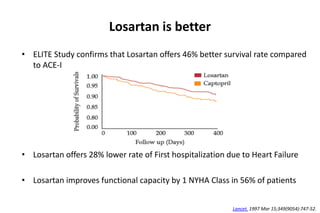
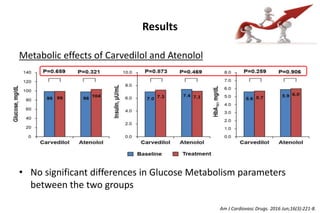
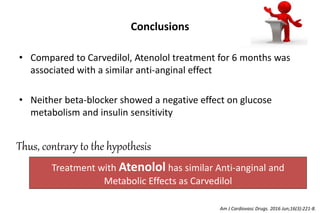
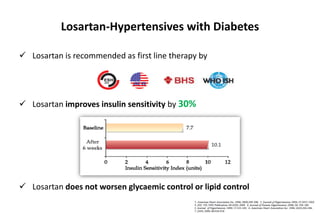
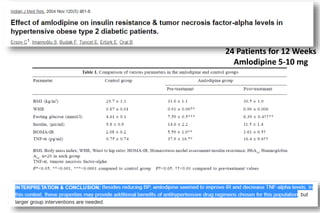
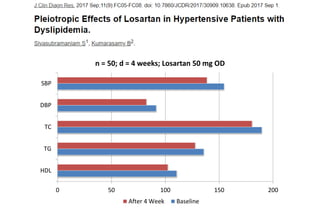
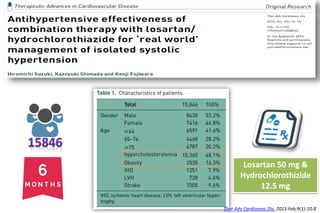
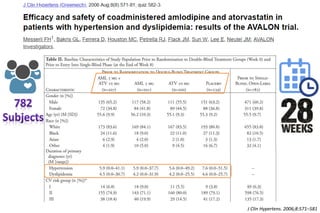
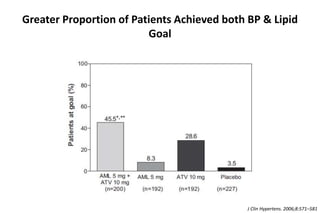
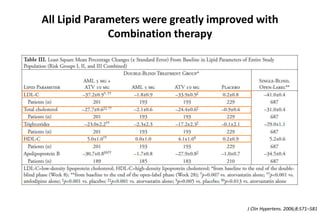
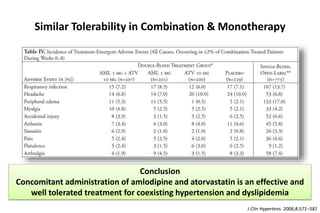
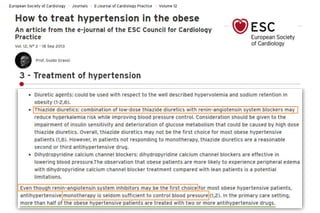
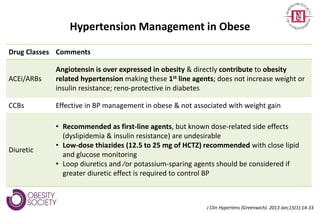
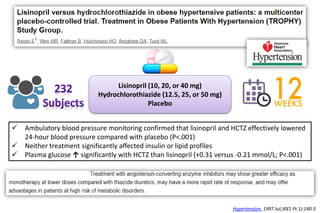
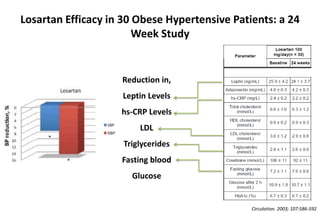
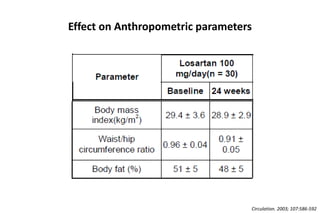
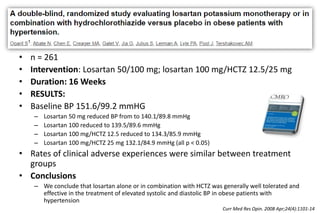
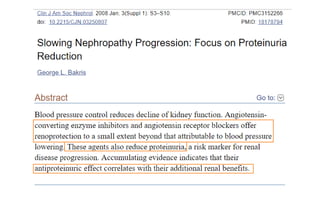
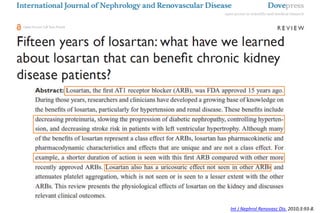
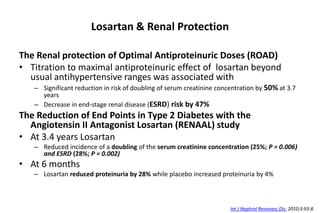
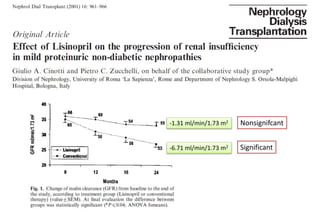
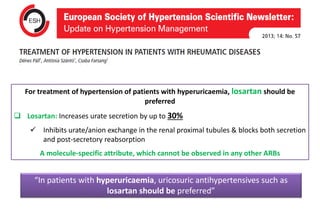
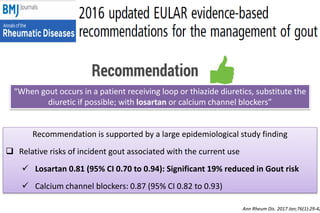
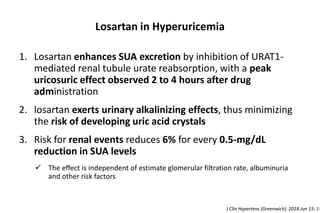
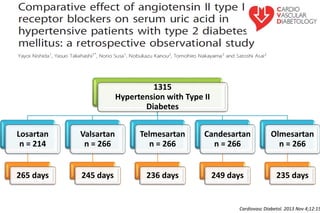
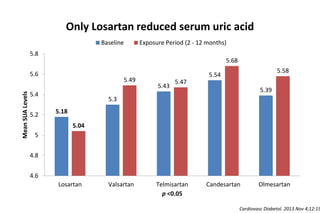
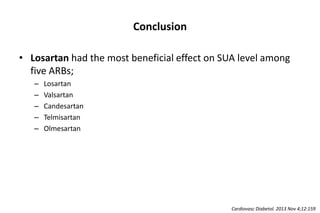
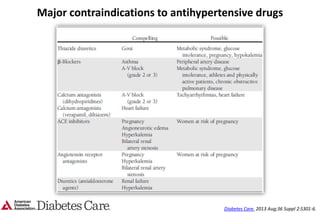
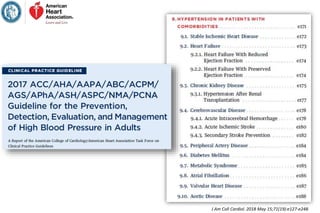
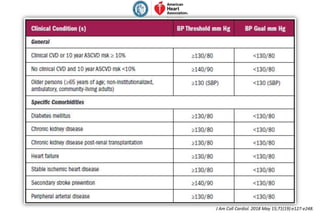
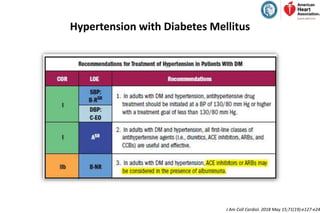
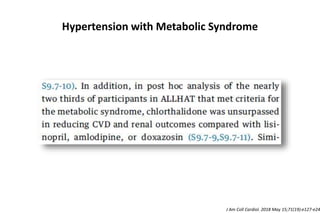
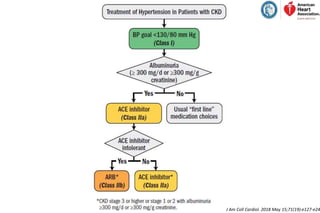
Hypertension is prevalent, especially in low and middle-income countries, with significant rates in regions like Russia (22% stage-I, 50% stage-II) and Africa (>40%). Coexisting conditions such as cardiovascular diseases, diabetes, and obesity are common among hypertensive patients, with elevated serum uric acid levels increasing the risk of cardiovascular events and mortality. Effective management strategies with medications like losartan and combination therapies have been shown to improve outcomes for patients with hypertension and associated comorbidities.