This document provides an overview of heart failure, including:
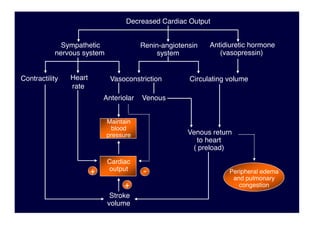
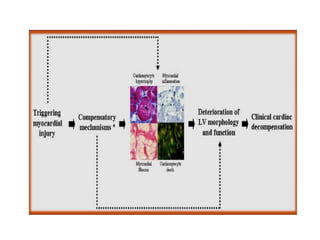
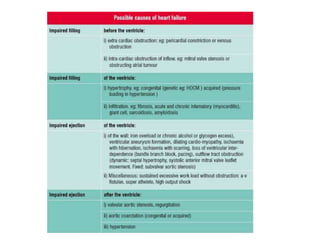
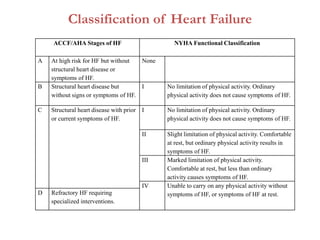
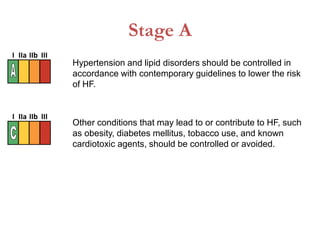
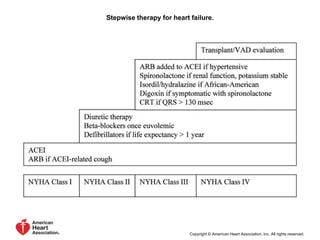
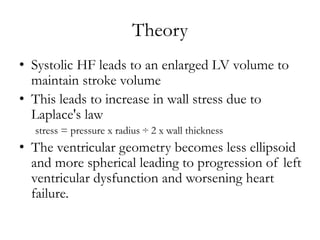
1. It defines heart failure and classifies it based on ACCF/AHA stages and NYHA functional classification.
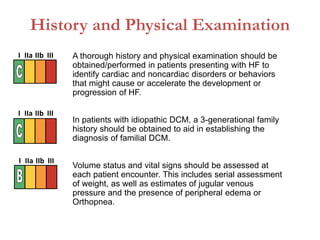
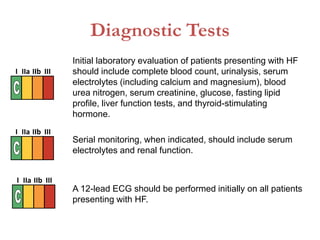
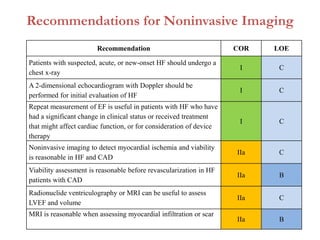
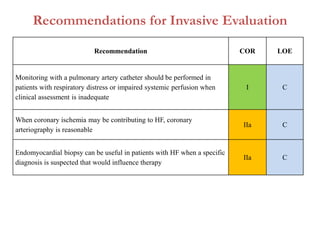
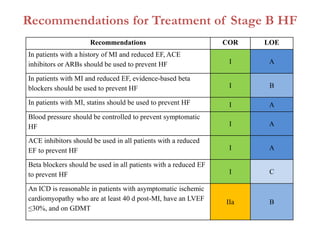
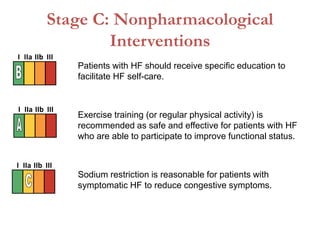
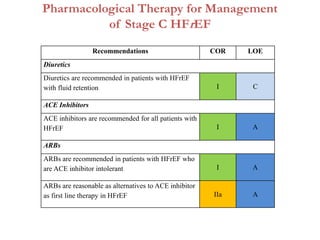
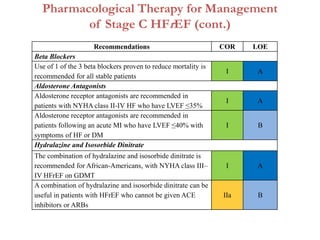
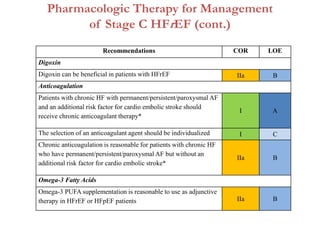
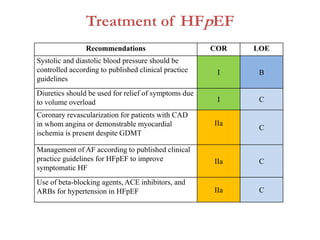
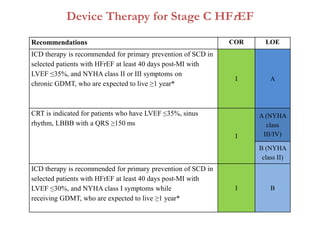
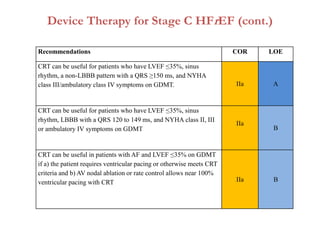
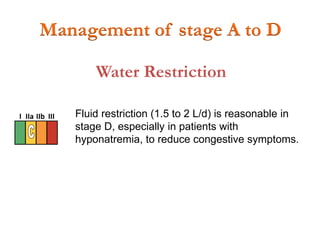
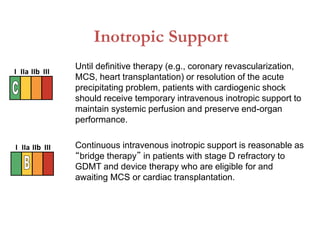
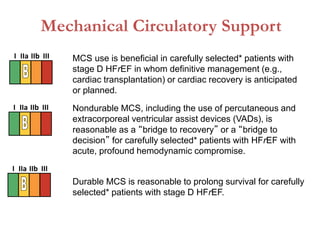
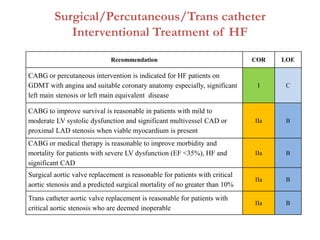
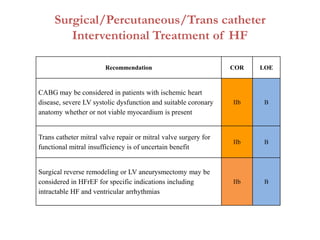
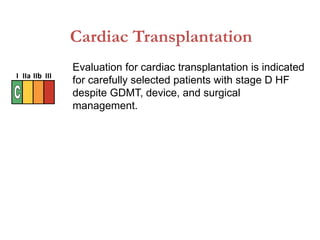
2. It outlines recommendations for diagnostic tests, noninvasive imaging, invasive evaluation, and pharmacological and nonpharmacological treatment for stages A through D.
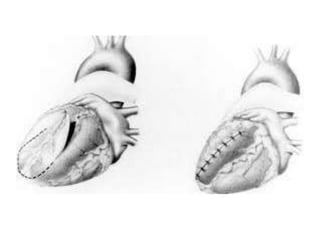
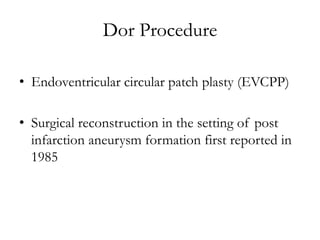
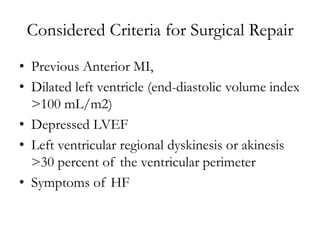
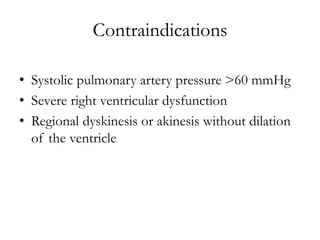
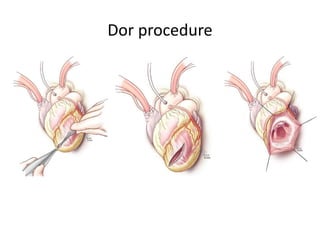
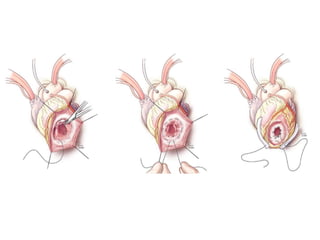
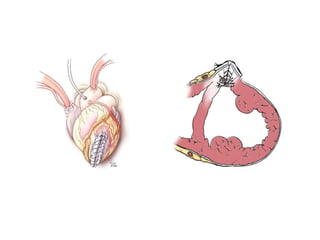
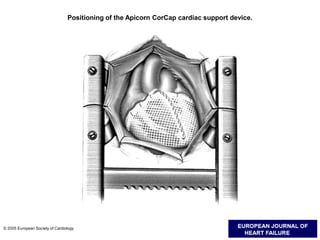
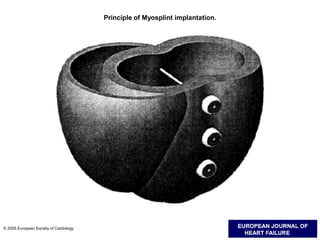
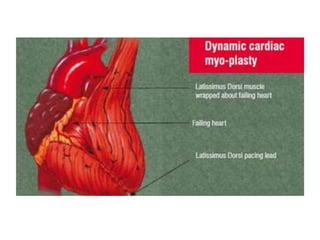
3. It discusses surgical interventions for heart failure such as ventricular reduction procedures, coronary artery bypass grafting, valve surgery, and cardiac transplantation.