1. The document summarizes a panel presentation on rural health equity and the social determinants of health at the 2011 Virginia Rural Health Summit.
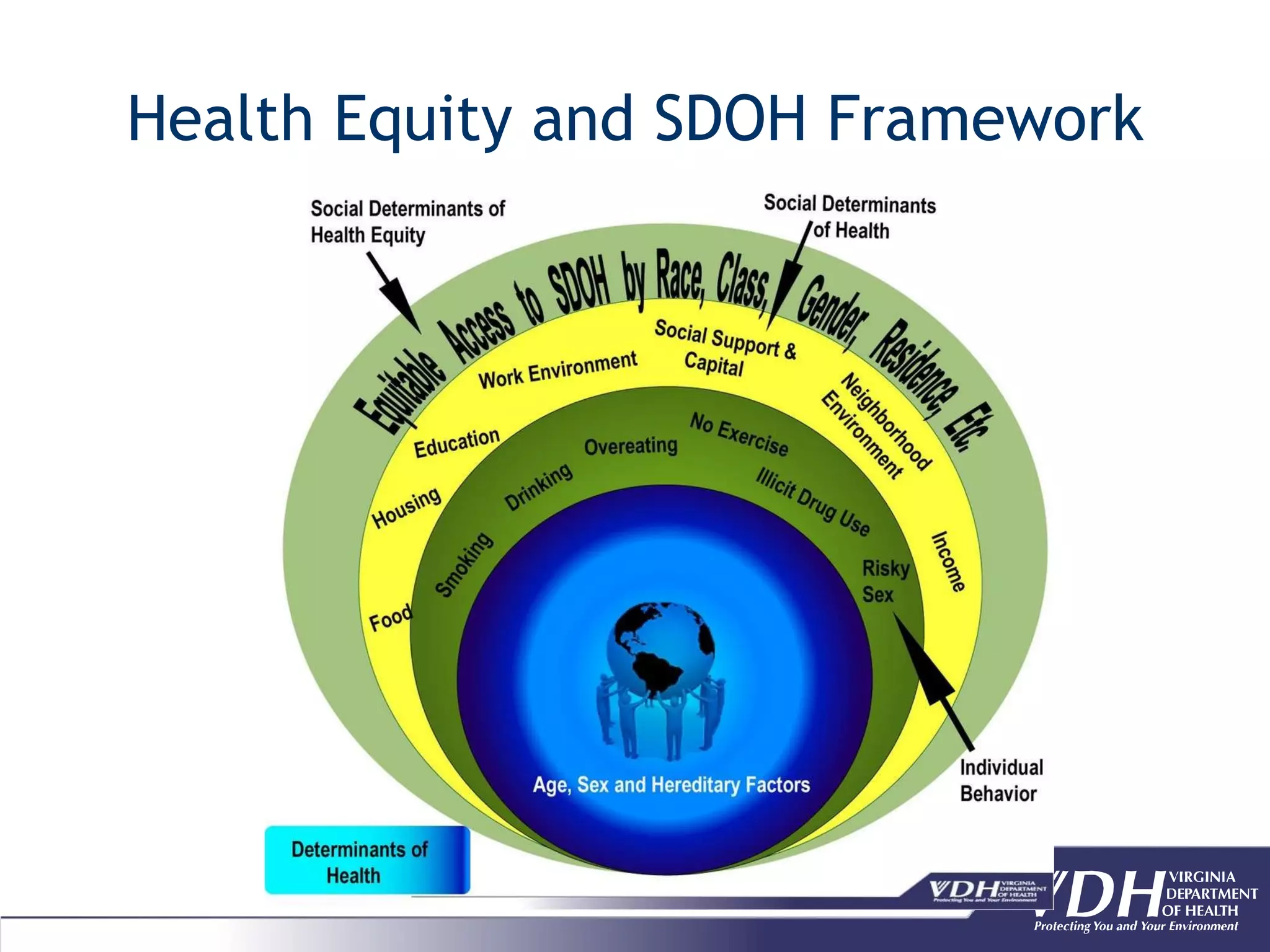
2. It defines key terms like health disparities and inequities, and describes a framework for health equity that focuses on equalizing conditions for health for all groups through addressing socioeconomic disadvantages and historical injustices.
3. Data on dimensions of health disparity and inequity in rural Virginia is presented, including comparisons between rural and non-rural areas, and differences by socioeconomic status, race/ethnicity, and gender.


![Definitions Health Disparities- “a population where there is a significant disparity [difference] in the overall rate of disease incidence, prevalence, morbidity, mortality, or survival rates in the population as compared to the health status of the general population.”- Minority Health and Health Disparities Research and Education Act, 2000 Health Inequities- “Disparities in health [or health care] that is systematic and avoidable and unjust.”- CDC](https://image.slidesharecdn.com/royster-final-110411201113-phpapp01/75/Health-Equity-3-2048.jpg)