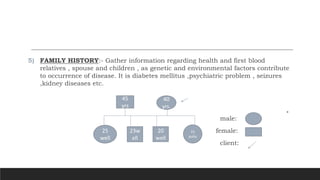
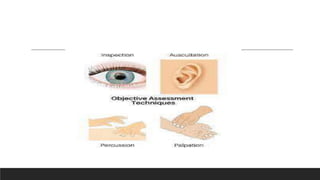
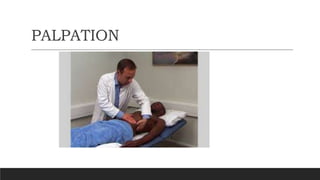
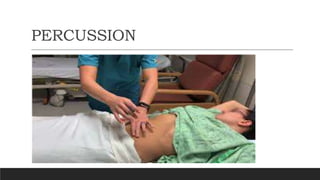
The document discusses health assessment, which involves collecting data about a client's health status through health history and physical examination. Health history gathers subjective and objective data through interviews and examinations. It covers biographical data, chief complaints, medical history, family history, and psychosocial history. Physical examination uses inspection, palpation, percussion, and auscultation to objectively evaluate body systems. Preparing the client and environment helps ensure a thorough yet comfortable assessment.