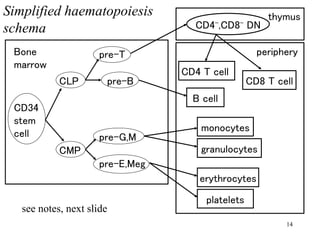
Haematopoiesis is the development of all blood cells from multipotent haematopoietic stem cells located in the bone marrow. Stem cells have the properties of self-renewal and potency to generate multiple cell types. They reside in a stem cell niche microenvironment that helps maintain their stemness. Upon division, one daughter stem cell remains in the niche while the other exits and becomes a transit cell. Transit cells amplify cell numbers through limited divisions before differentiating into functional end cells. There are two intermediate progenitor cells - common lymphoid progenitors that generate lymphocytes, and common myeloid progenitors that generate other blood cell types including erythrocytes and platelets. Haematopoies