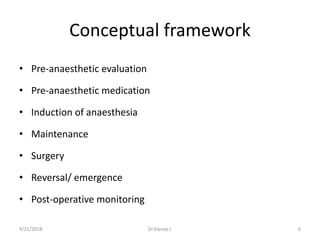
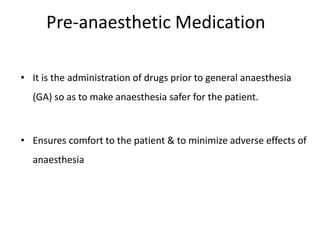
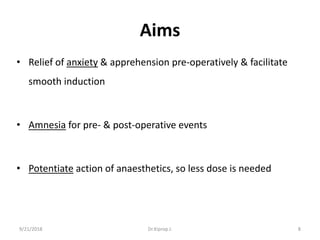
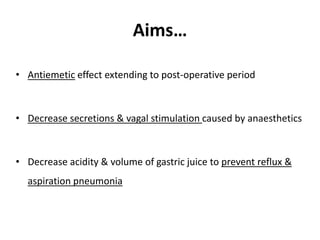
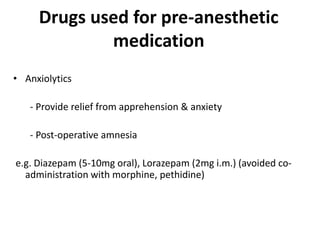
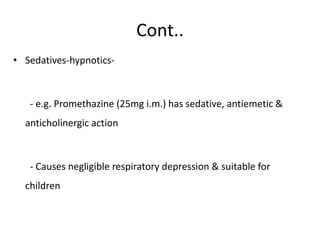
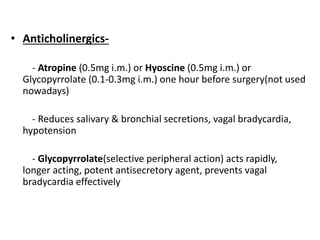
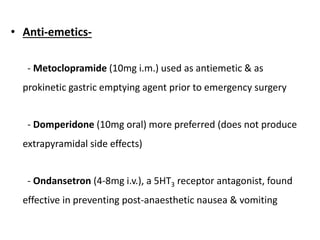
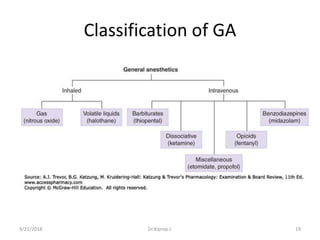
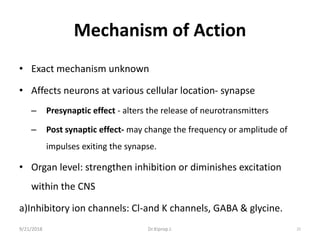
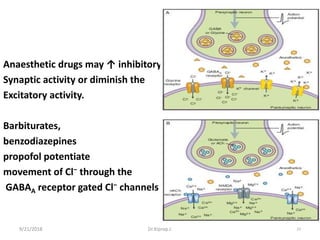
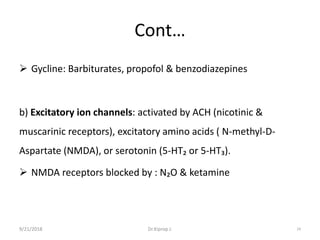
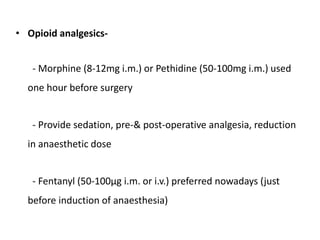
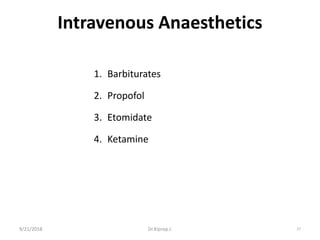
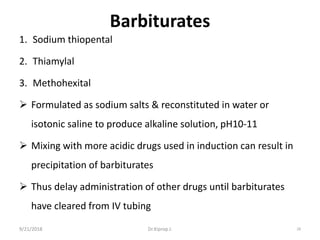
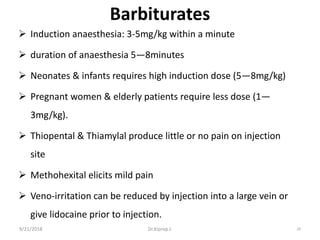
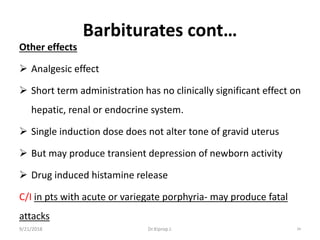
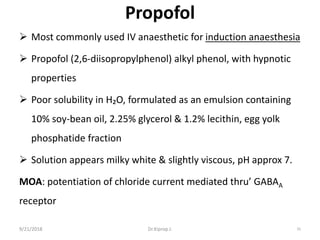
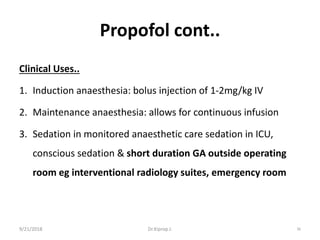
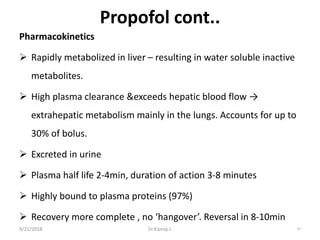
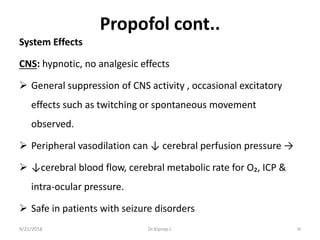
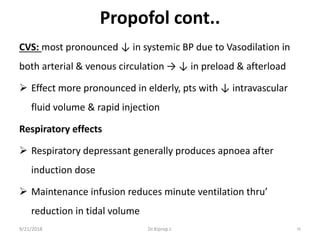
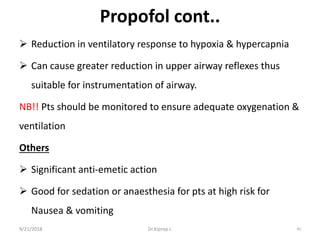
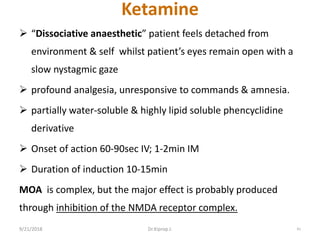
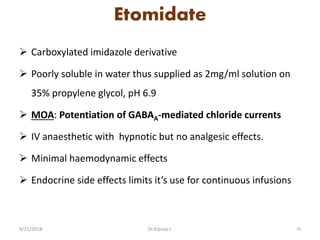
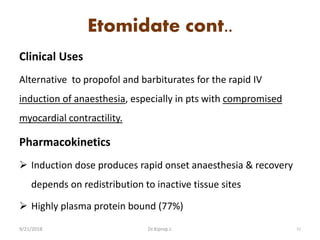
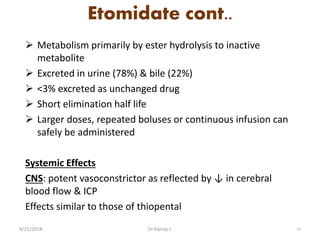
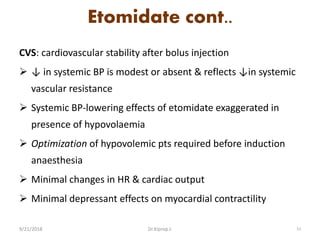
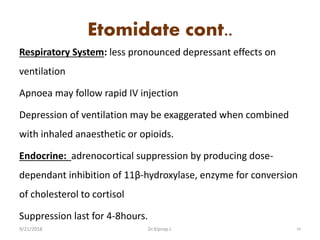
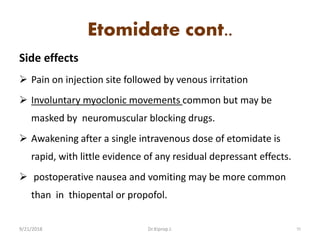
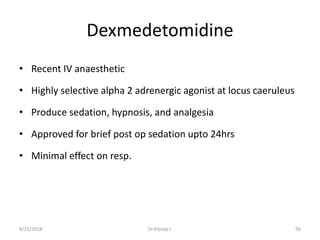
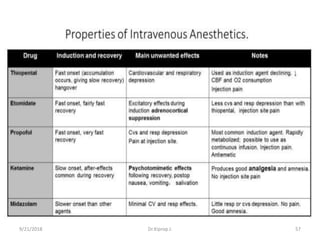
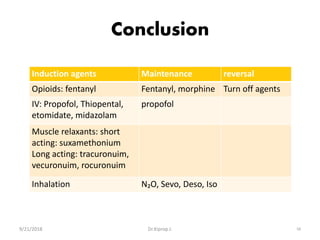
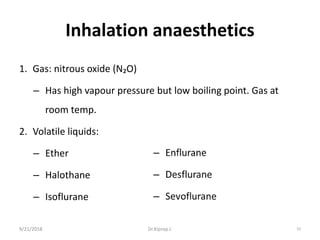
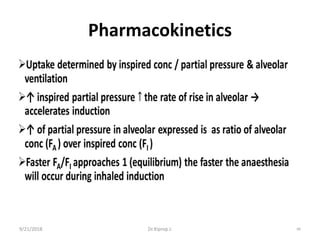
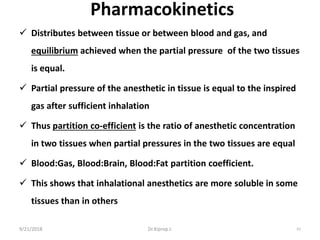
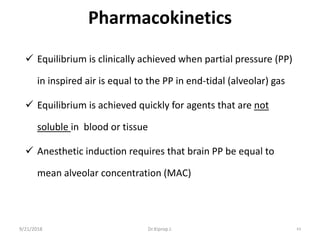
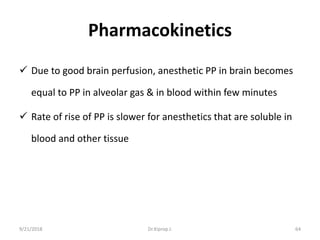
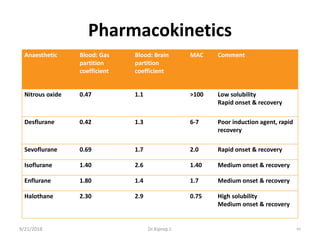
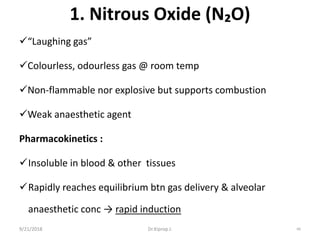
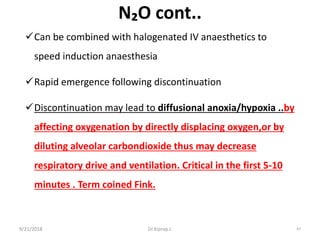
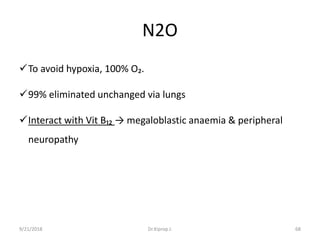
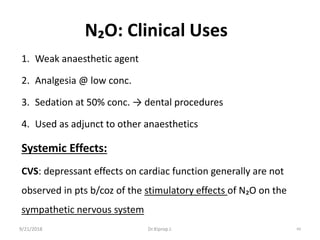
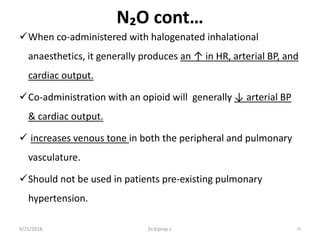
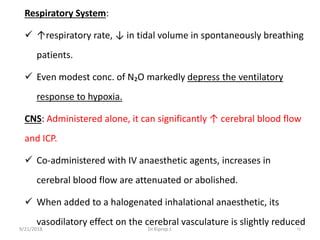
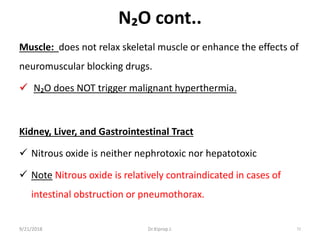
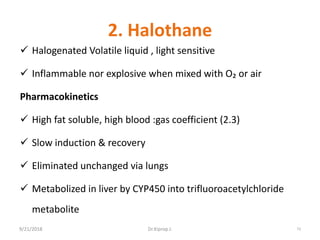
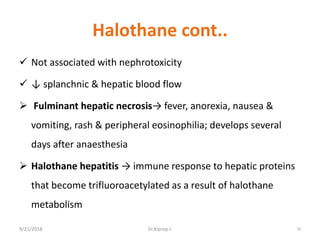
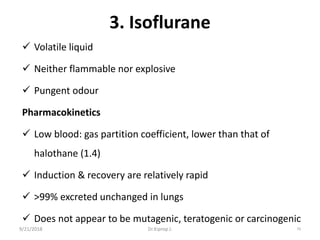
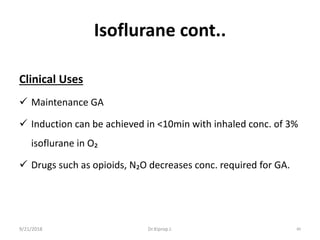
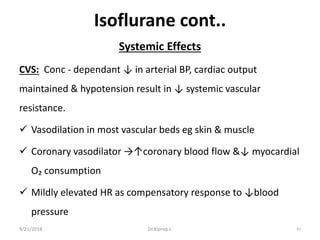
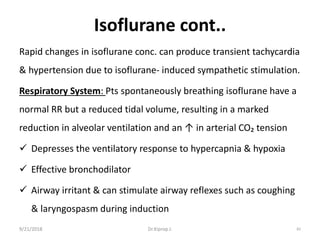
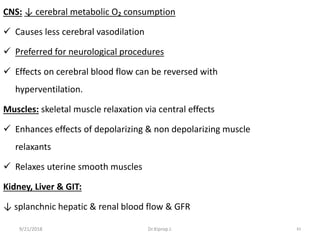
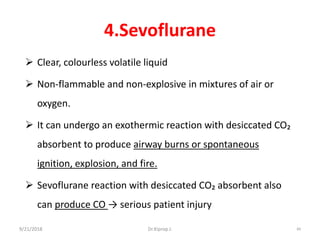
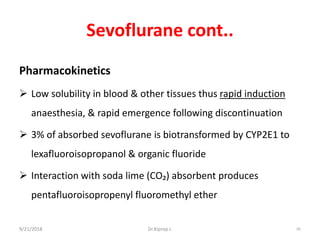
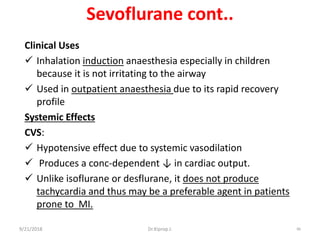
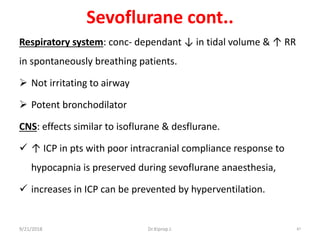
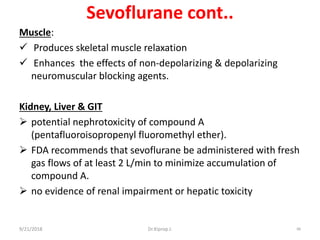
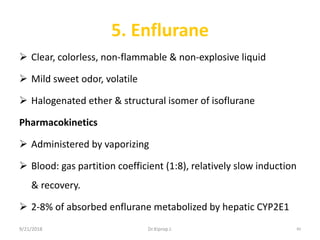
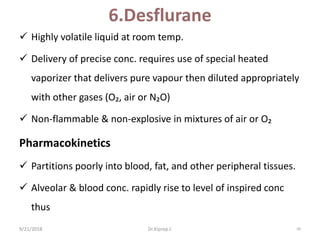
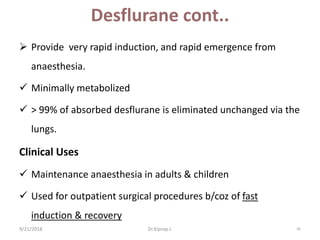
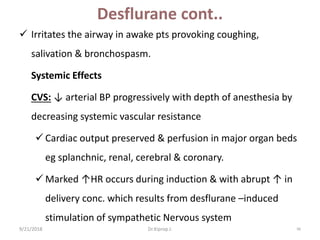
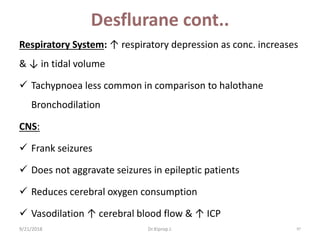
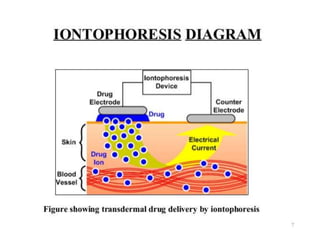
This document discusses general and local anesthetics. It provides an overview of pre-anesthetic medications that are given before general anesthesia to reduce anxiety, provide amnesia and potentiate the effects of anesthetics. It also describes various inhalation anesthetics like nitrous oxide and intravenous anesthetics such as barbiturates, propofol, etomidate and ketamine. It discusses the mechanisms of action, clinical uses and effects of these anesthetics on different body systems.