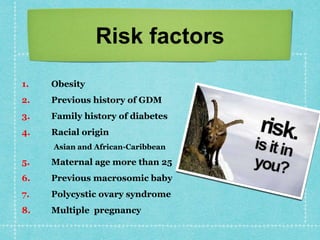
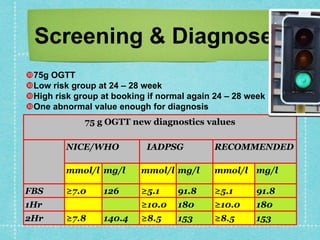
Gestational diabetes is glucose intolerance first recognized during pregnancy. It occurs due to placental hormones causing insulin resistance. Risk factors include obesity, family history of diabetes, and advanced maternal age. It is screened for and diagnosed using a 75g oral glucose tolerance test. Treatment involves lifestyle modifications like diet and exercise as well as insulin therapy if needed. Close monitoring of blood glucose and fetal well-being is required. Management aims to prevent complications in both mother and baby.