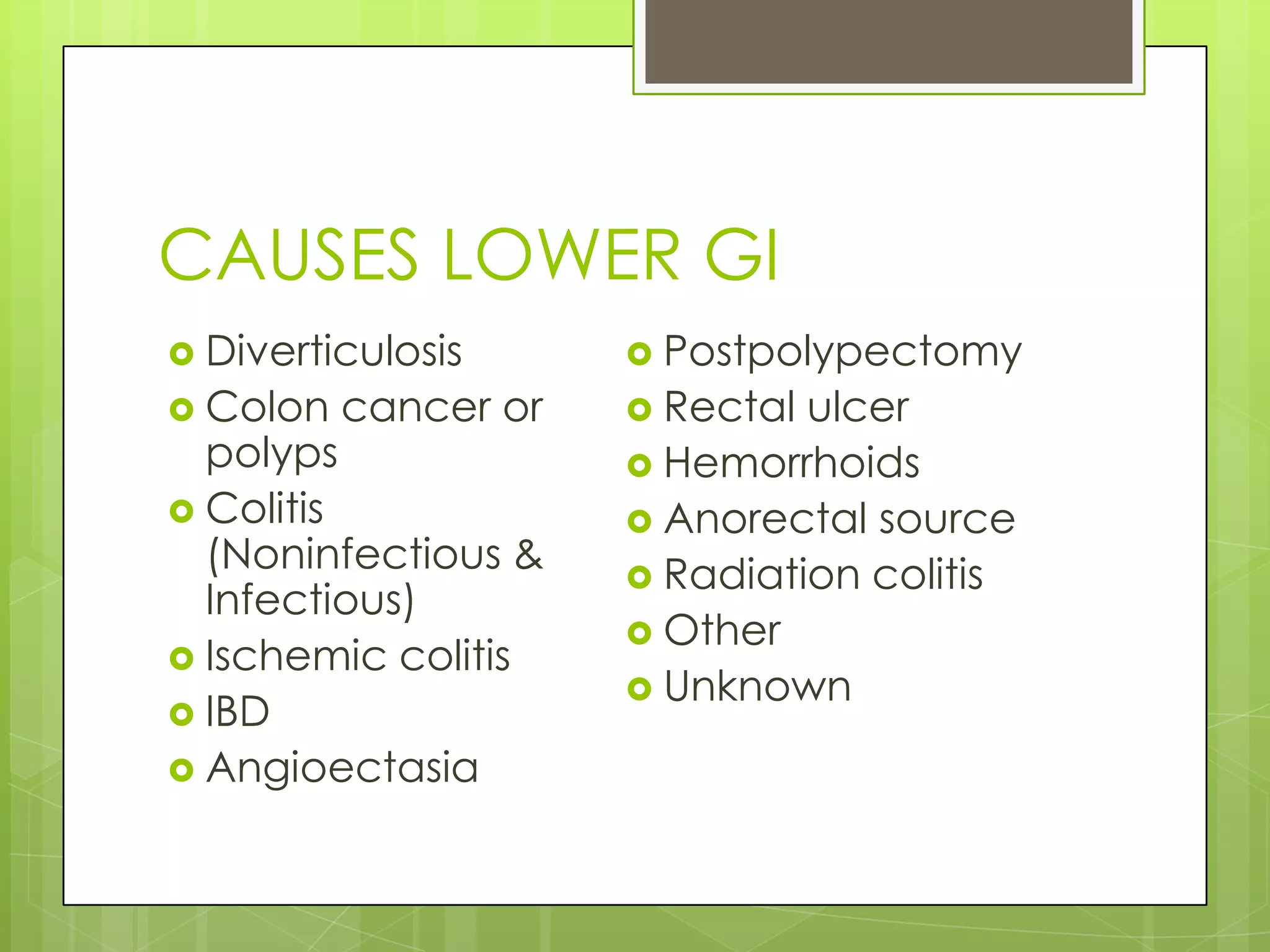
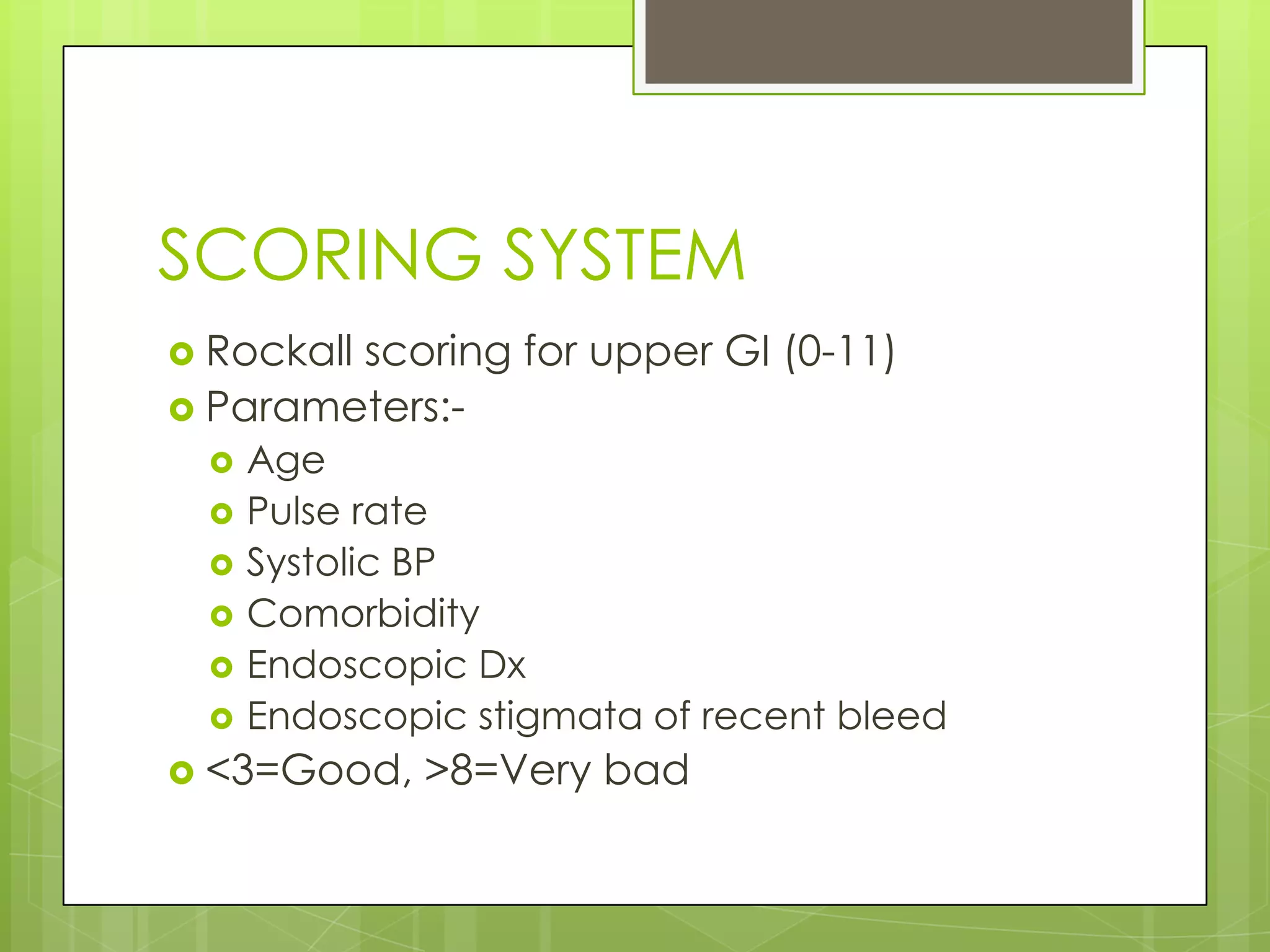
This document discusses gastrointestinal (GI) bleeding, including its definitions, symptoms, causes, management, and prevention. GI bleeding can occur in the upper or lower GI tract, and may present as vomiting blood, black stools, or blood in the rectum. Common causes include peptic ulcers, esophageal varices, colon polyps, and diverticulosis. Management involves stabilizing the patient, stopping the bleeding, identifying the source of bleeding, and preventing recurrence. Endoscopy allows for diagnosis and potential treatment through procedures like ligation or sclerosing of varices. Surgery may be considered for severe or recurrent bleeding. Scoring systems can help determine prognosis and appropriate care settings.