This document discusses various types of crystal-associated arthropathies including:
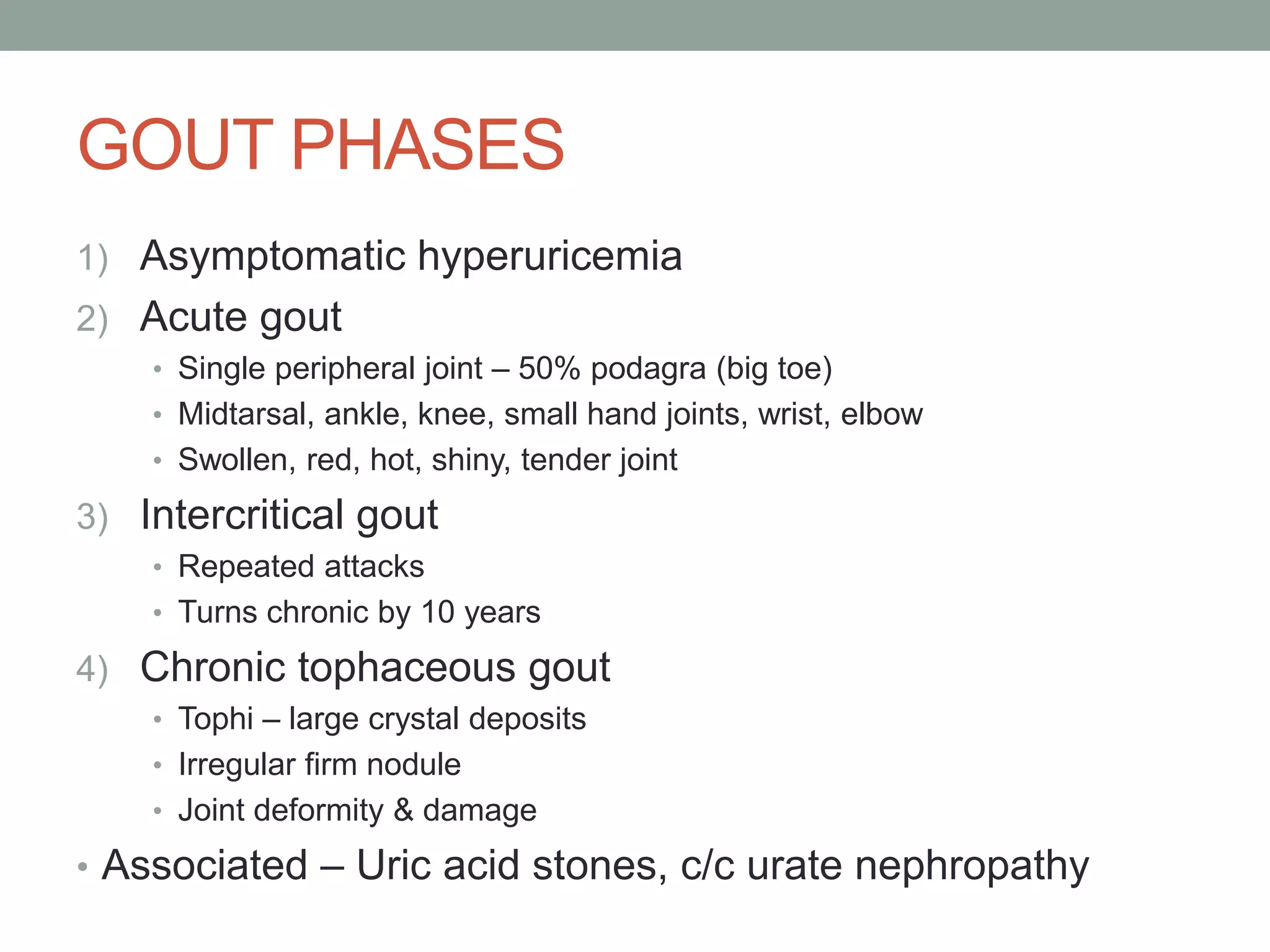
- Monosodium urate monohydrate crystals which cause gout. Gout typically affects middle-aged males and causes painful inflammation in joints.
- Calcium pyrophosphate dihydrate crystals which cause pseudogout/chondrocalcinosis. This tends to affect the elderly and can mimic many other joint diseases.
- Calcium-containing crystals like hydroxyapatite which are associated with aging, osteoarthritis, and renal disease and can cause acute attacks of inflammation.