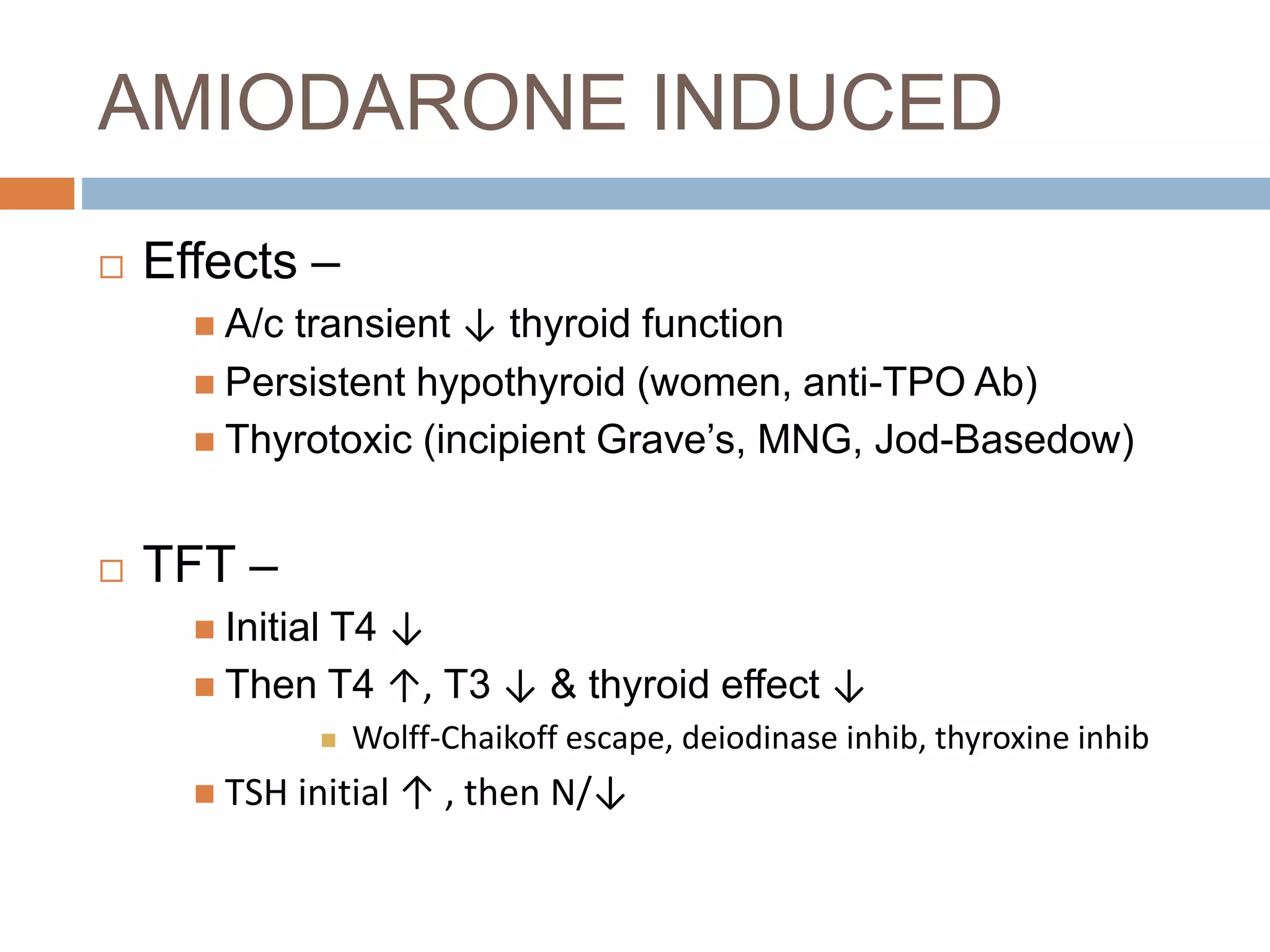
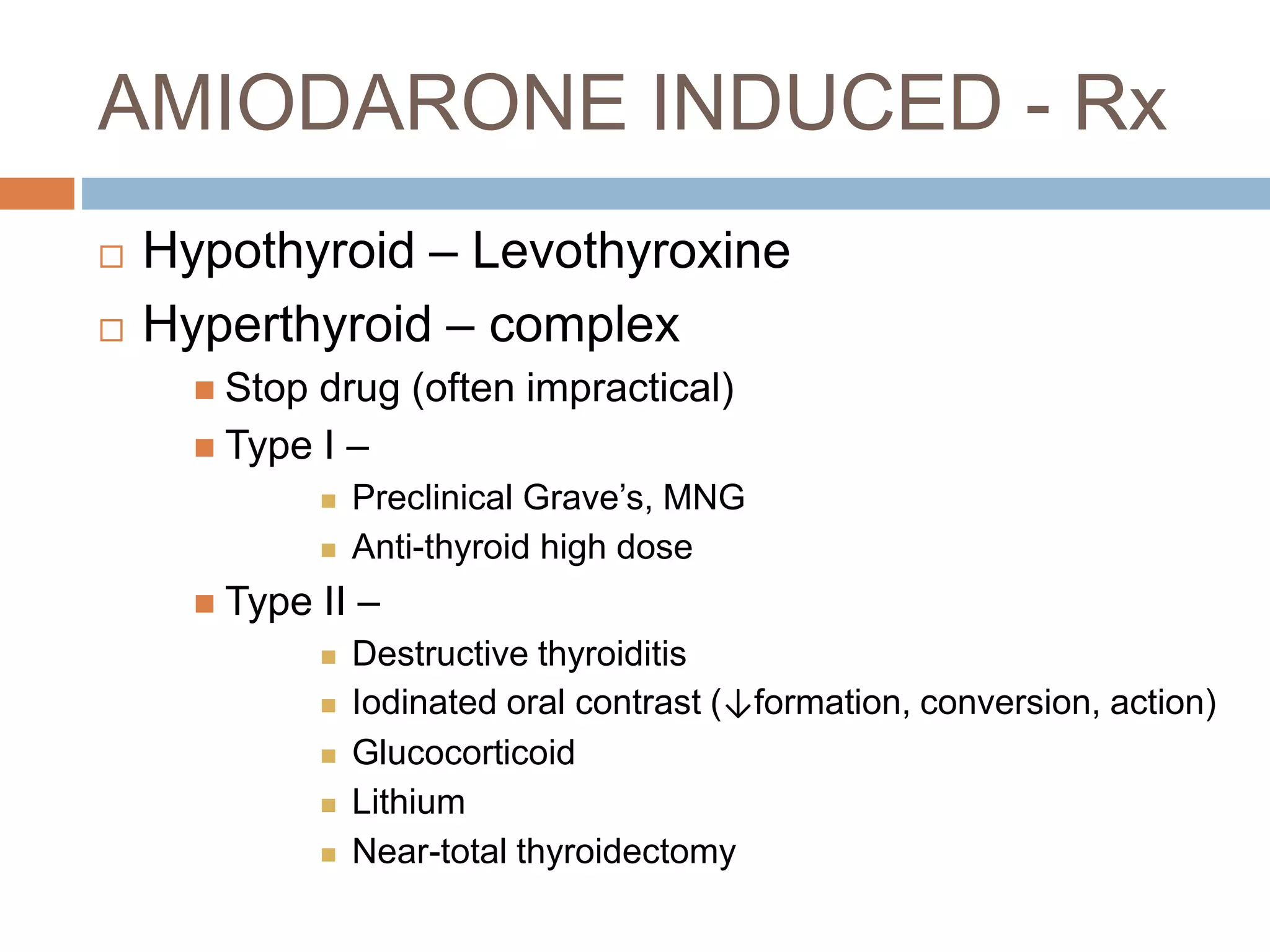
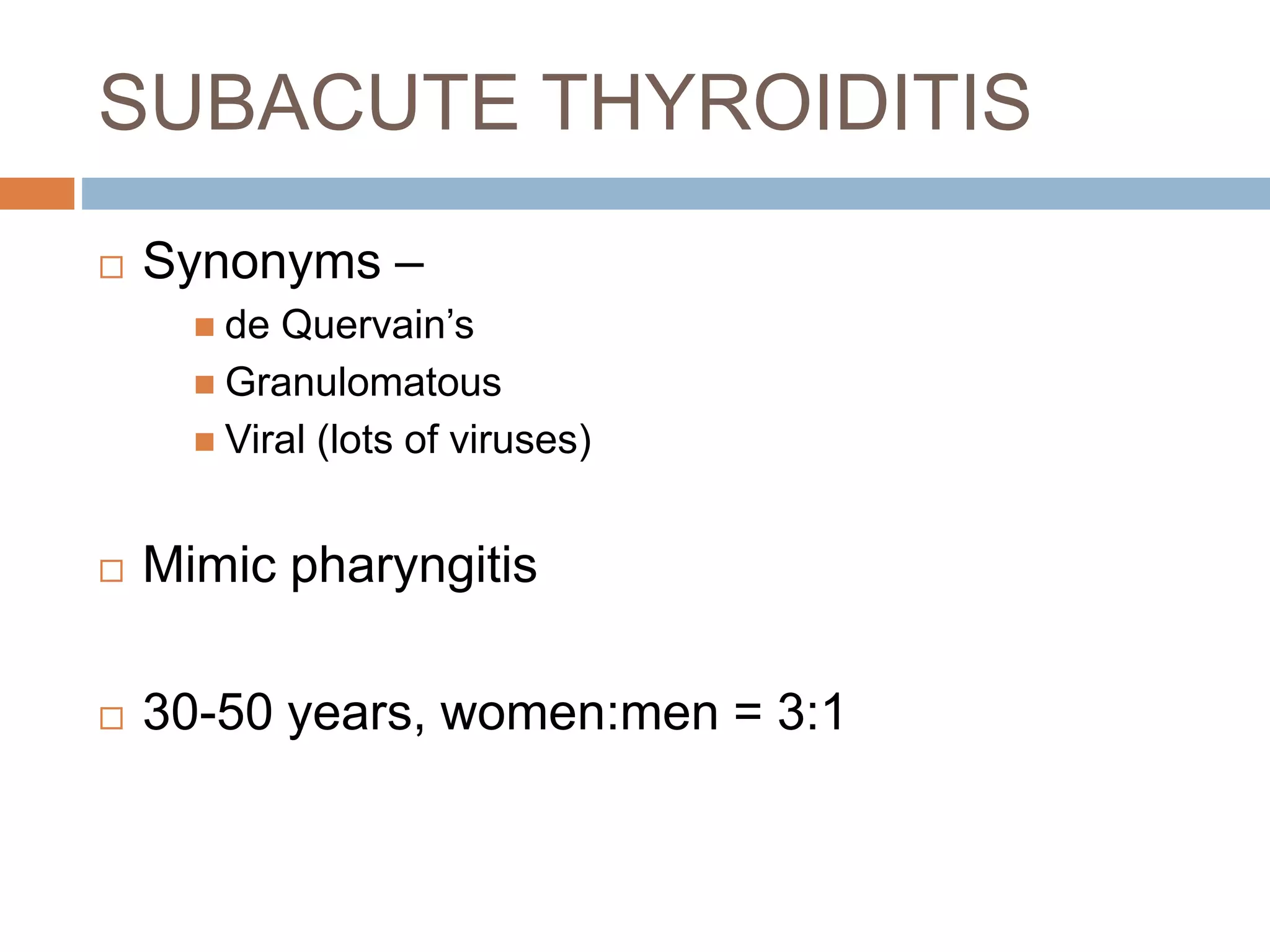
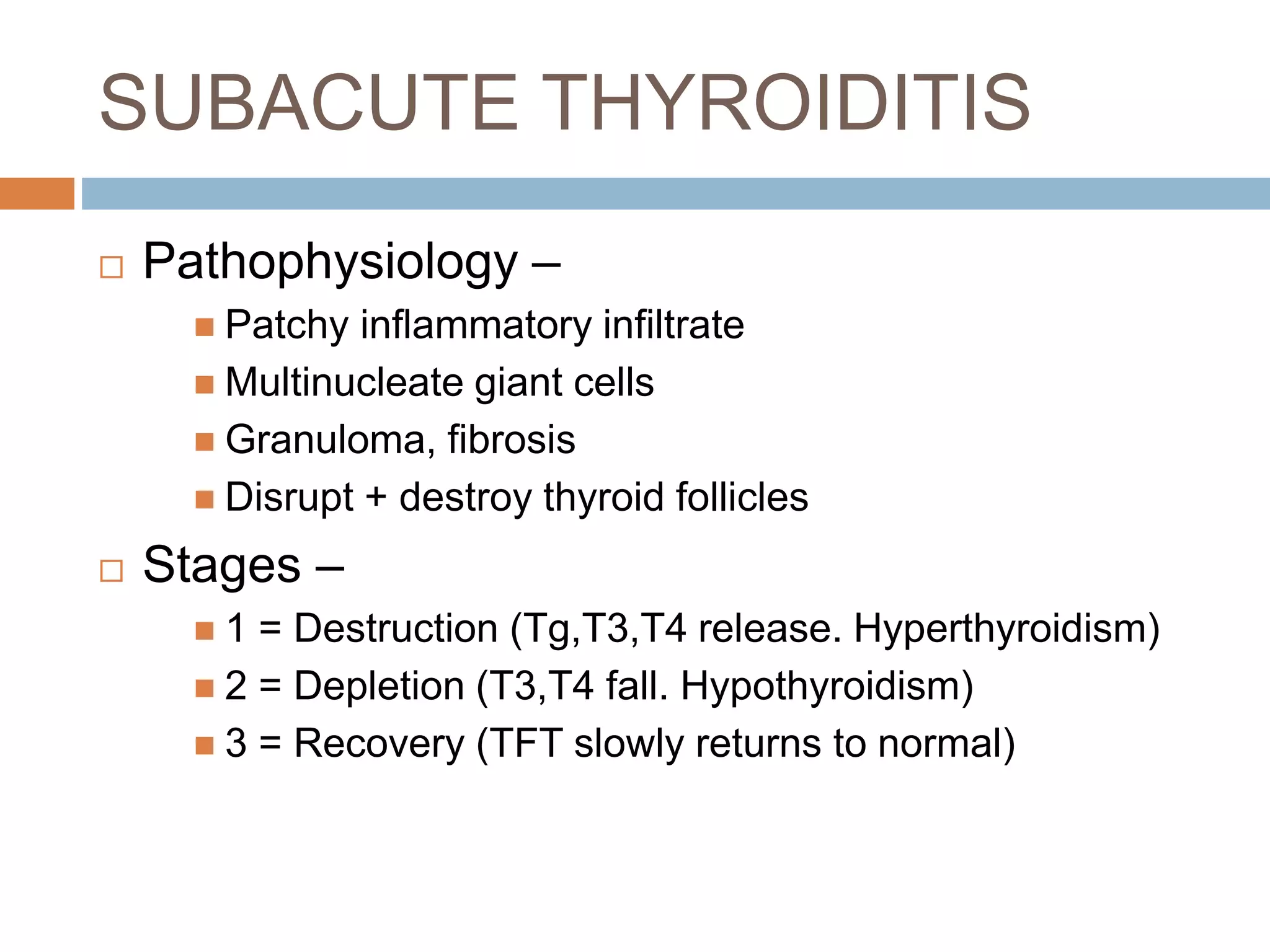
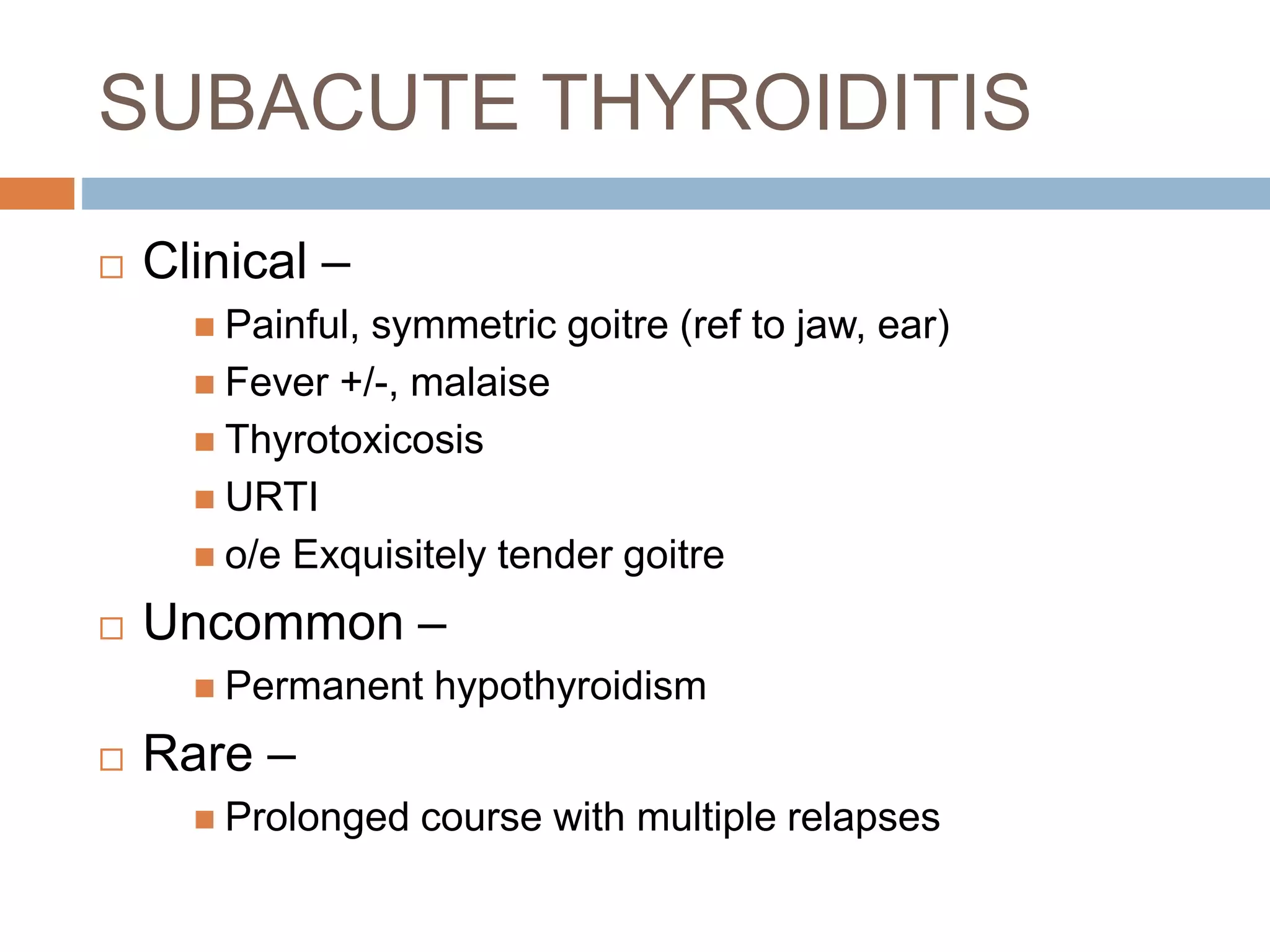
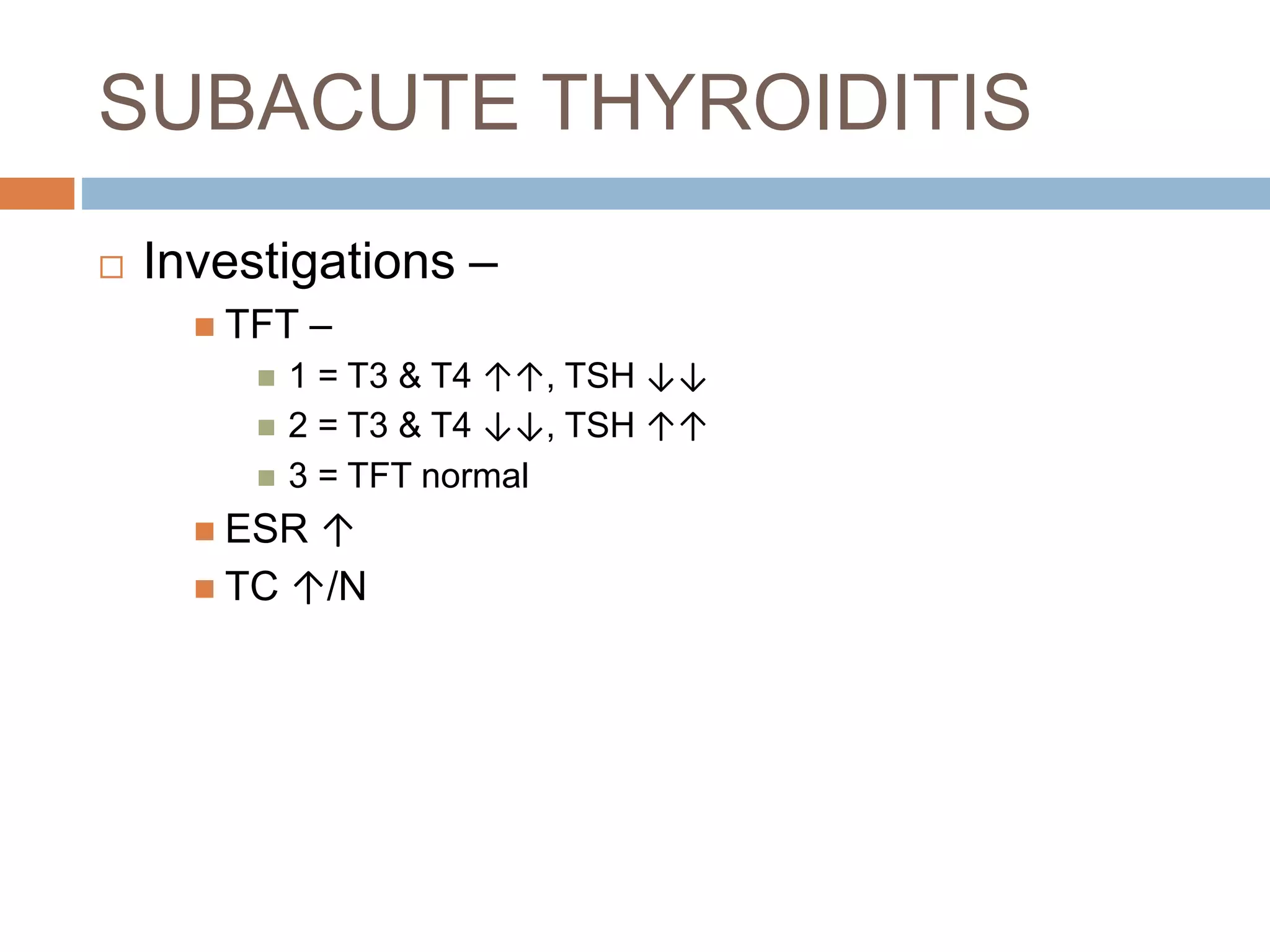
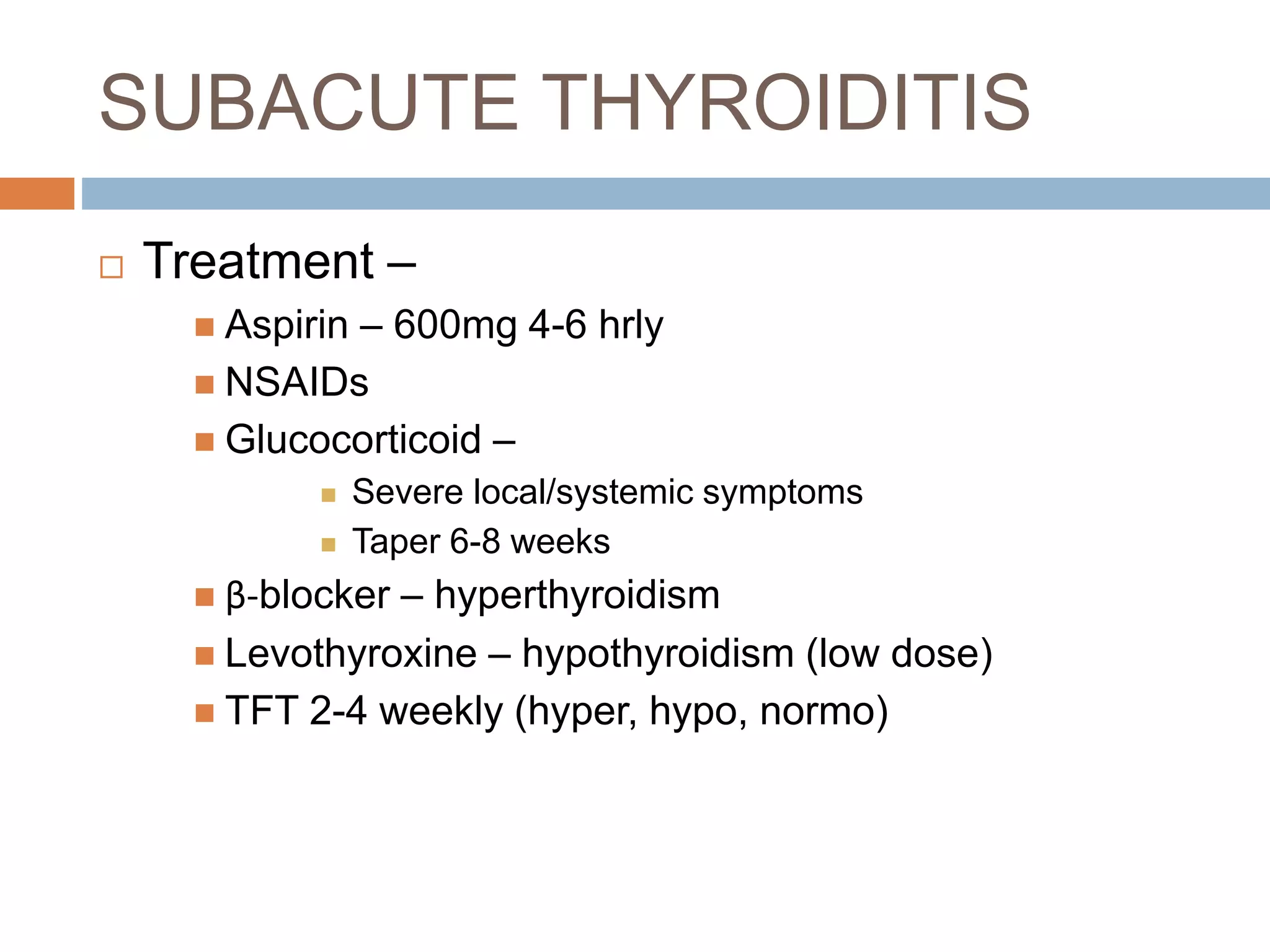
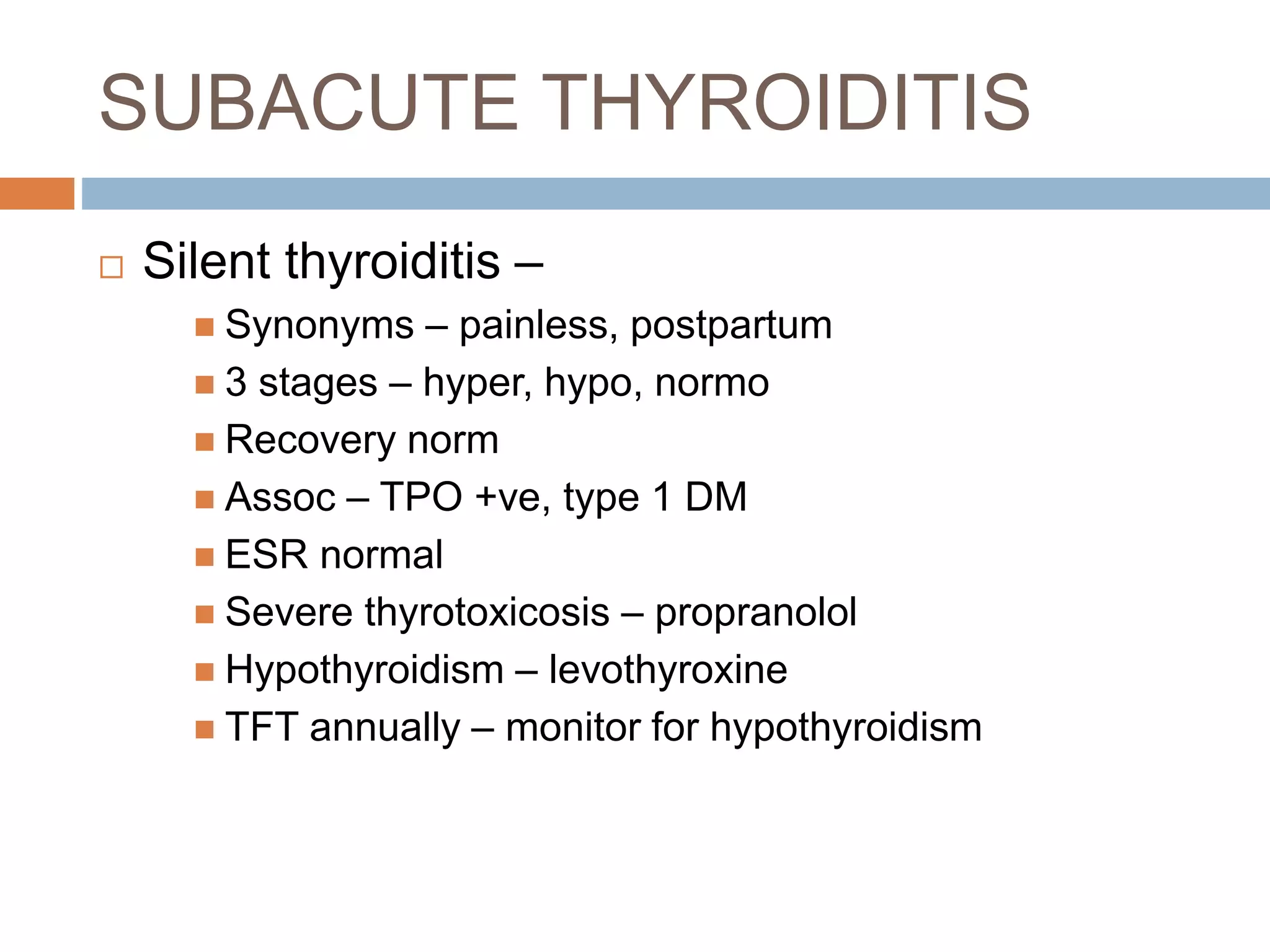
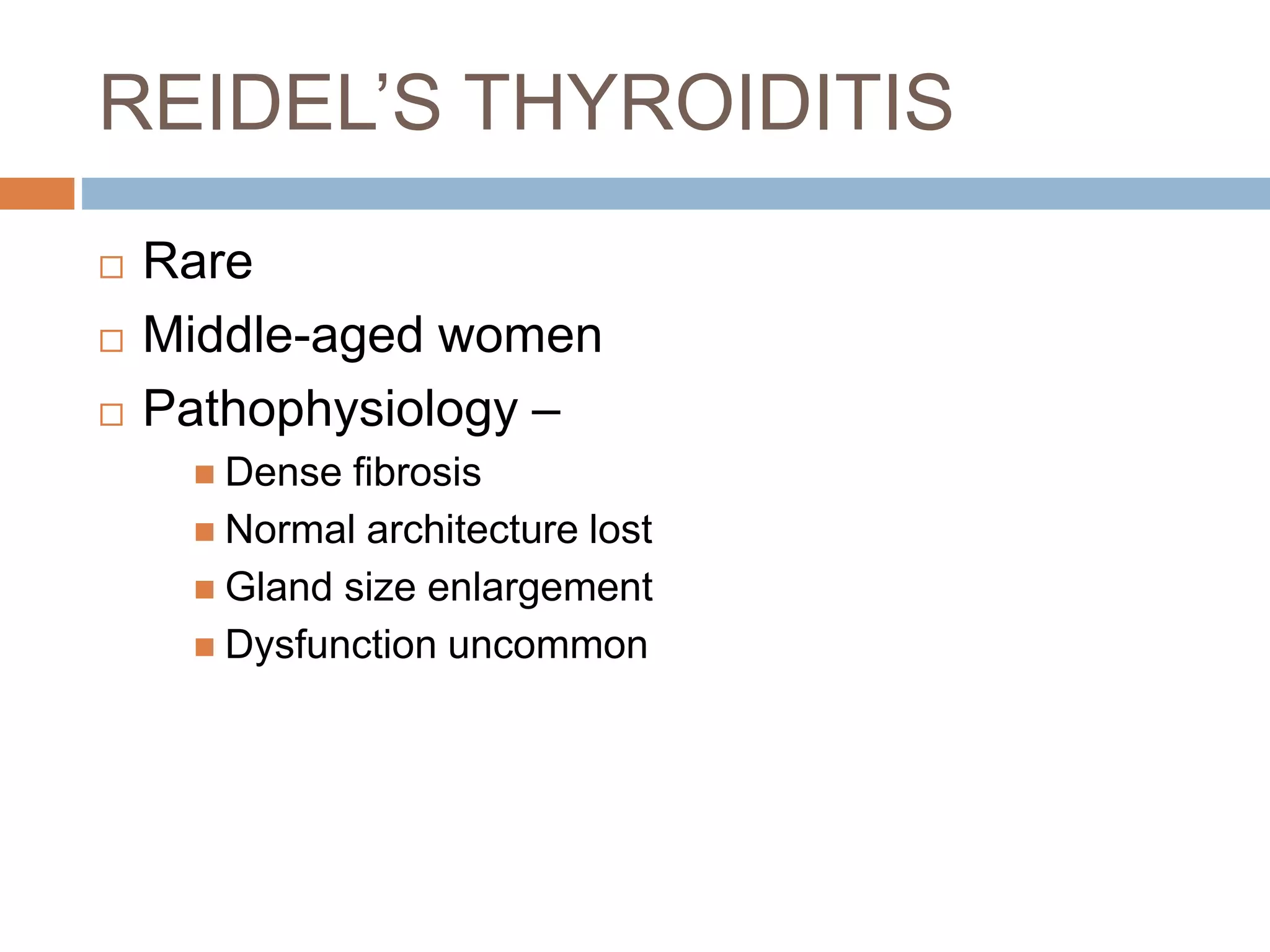
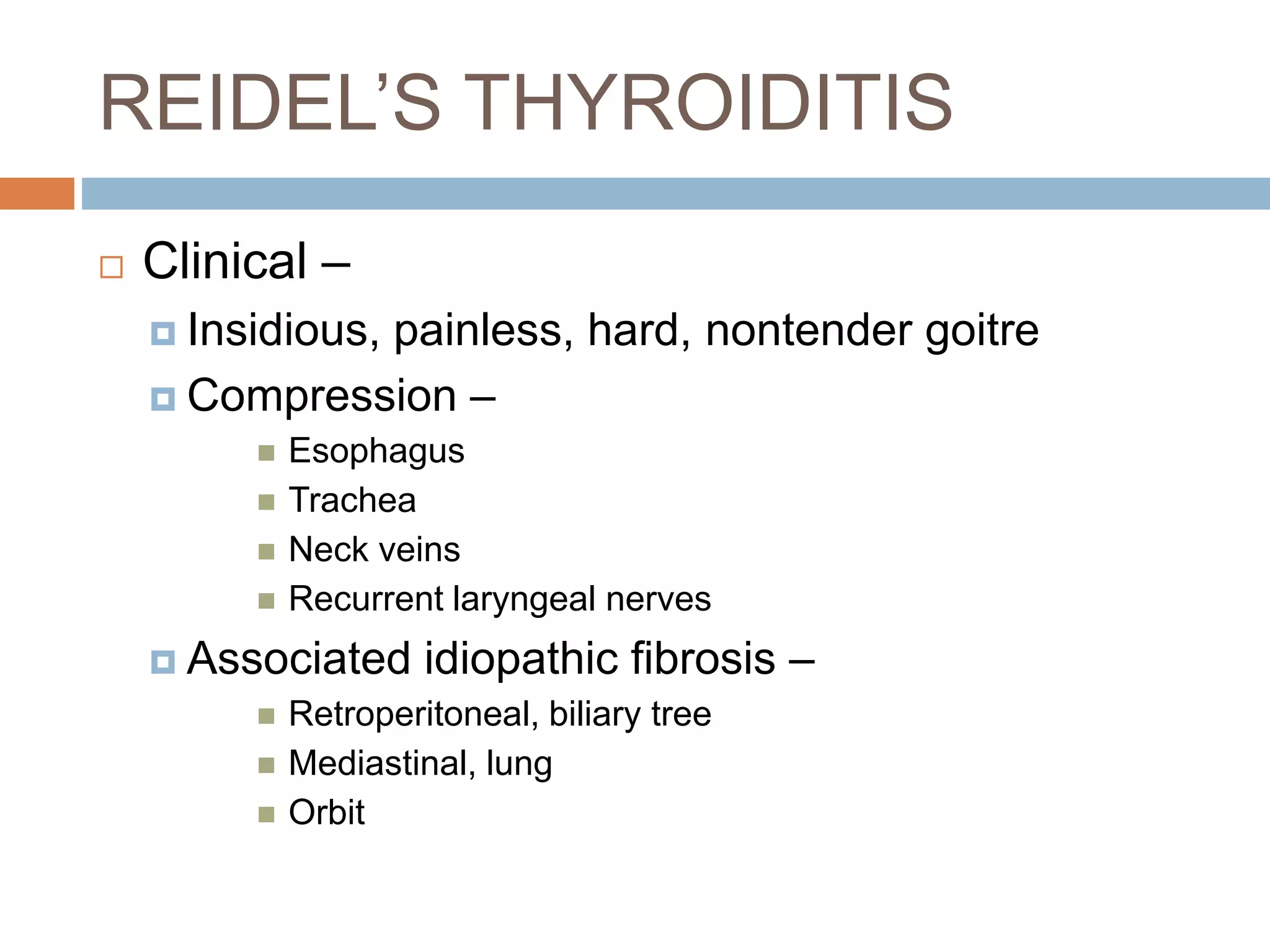
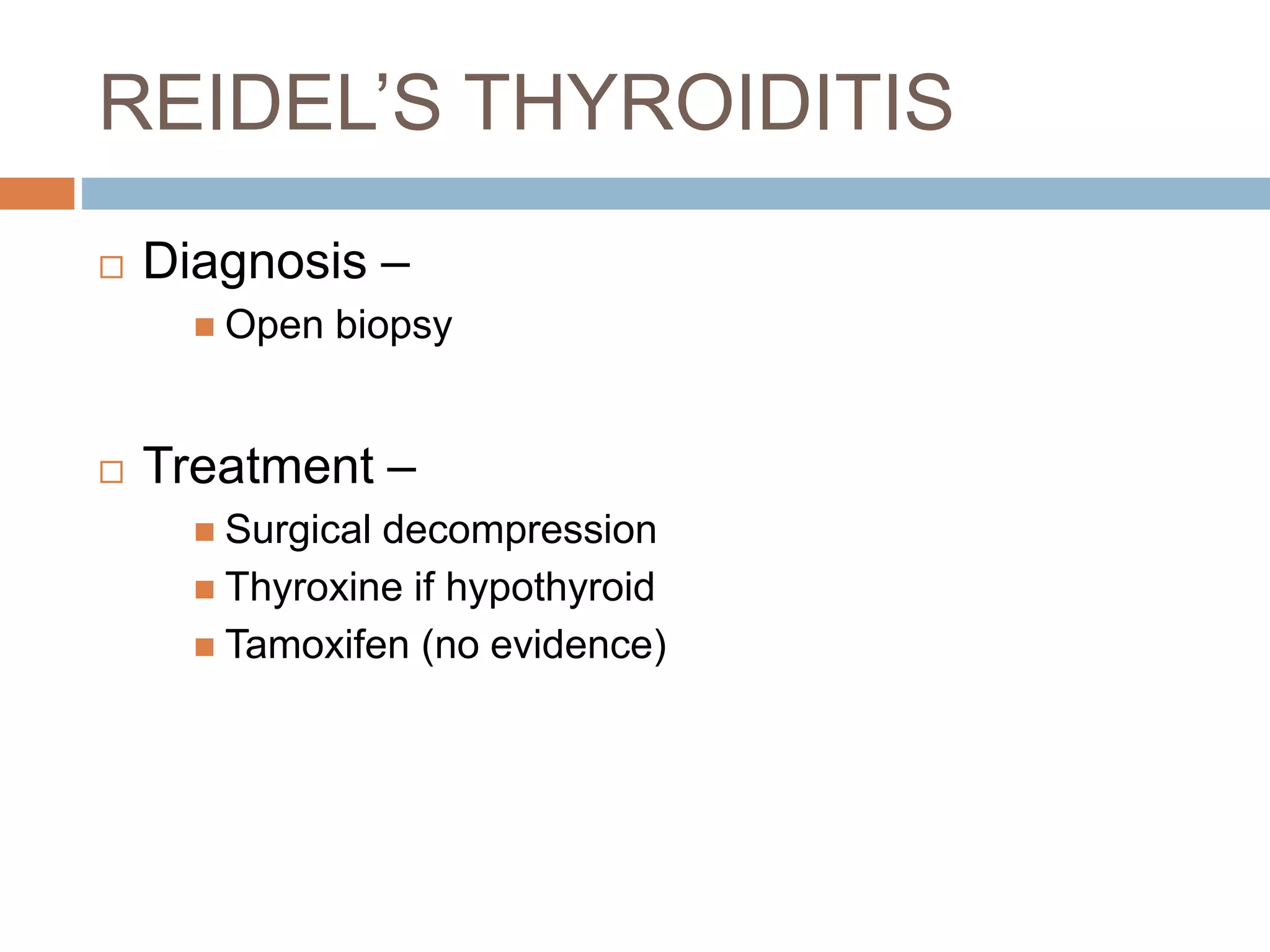
This document discusses various types of thyroid disorders including simple goiter, thyroiditis, drug-induced thyroiditis, and autoimmune thyroiditis. Simple goiter is usually asymptomatic and caused by iodine deficiency or goitrogen intake. Thyroiditis can be acute from infections, subacute from viruses, or chronic from autoimmunity. Drug-induced thyroiditis is caused by medications like amiodarone and interferons. Autoimmune thyroiditis involves lymphocytic infiltration and can lead to hypothyroidism.