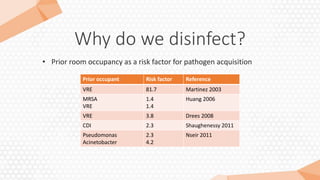
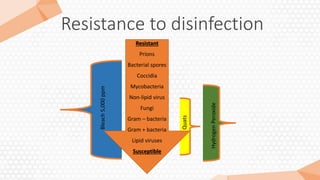
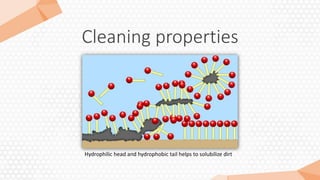
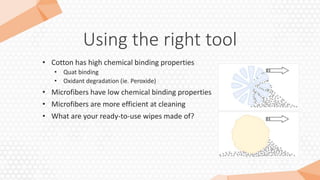
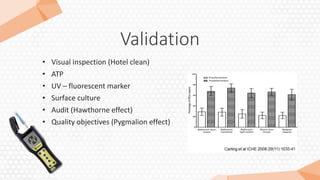
The document outlines the critical aspects of preventing healthcare-associated infections (HAIs) through effective environmental hygiene practices. It highlights the significant burden of HAIs in Canada, emphasizing the importance of disinfection, proper product use, and training for personnel involved in infection control. Additionally, it reviews best practices, challenges like Clostridium difficile, and validation procedures to ensure efficacy in disinfection efforts.