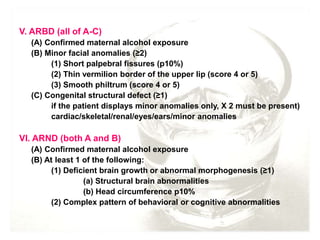
This document discusses alcohol intake during pregnancy and fetal alcohol spectrum disorders (FASD). It provides statistics on alcohol use during pregnancy from various studies. It notes that a safe level of alcohol during pregnancy has not been determined, as the effects of alcohol on the fetus are variable depending on factors like the mother's metabolism and drinking patterns. Low to moderate prenatal alcohol exposure has not shown effects in some studies, but other research has found children with FAS even with reported low alcohol intake. The document describes clinical features of FASD including facial abnormalities, growth issues, central nervous system anomalies, and functional impairments. It discusses diagnostic criteria from various organizations and guidelines for diagnosing FASD.