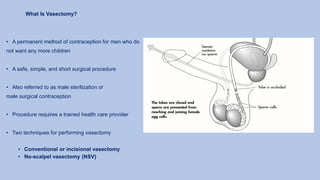
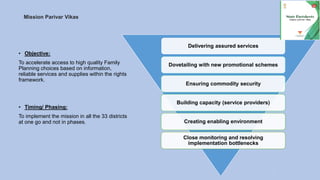
This document discusses family planning, its importance, and various methods. It summarizes family planning status in Assam based on NFHS-5 data, including current usage of different methods. The importance of family planning is outlined, such as improving maternal and child health, preventing unintended pregnancies and unsafe abortions, empowering women, and promoting social and economic development. National population policy objectives are presented. The document then describes various family planning methods available in India, including temporary and permanent methods. Effectiveness, use, and mechanisms of different methods like pills, IUCDs, sterilization procedures are explained. The importance of quality family planning services is emphasized.