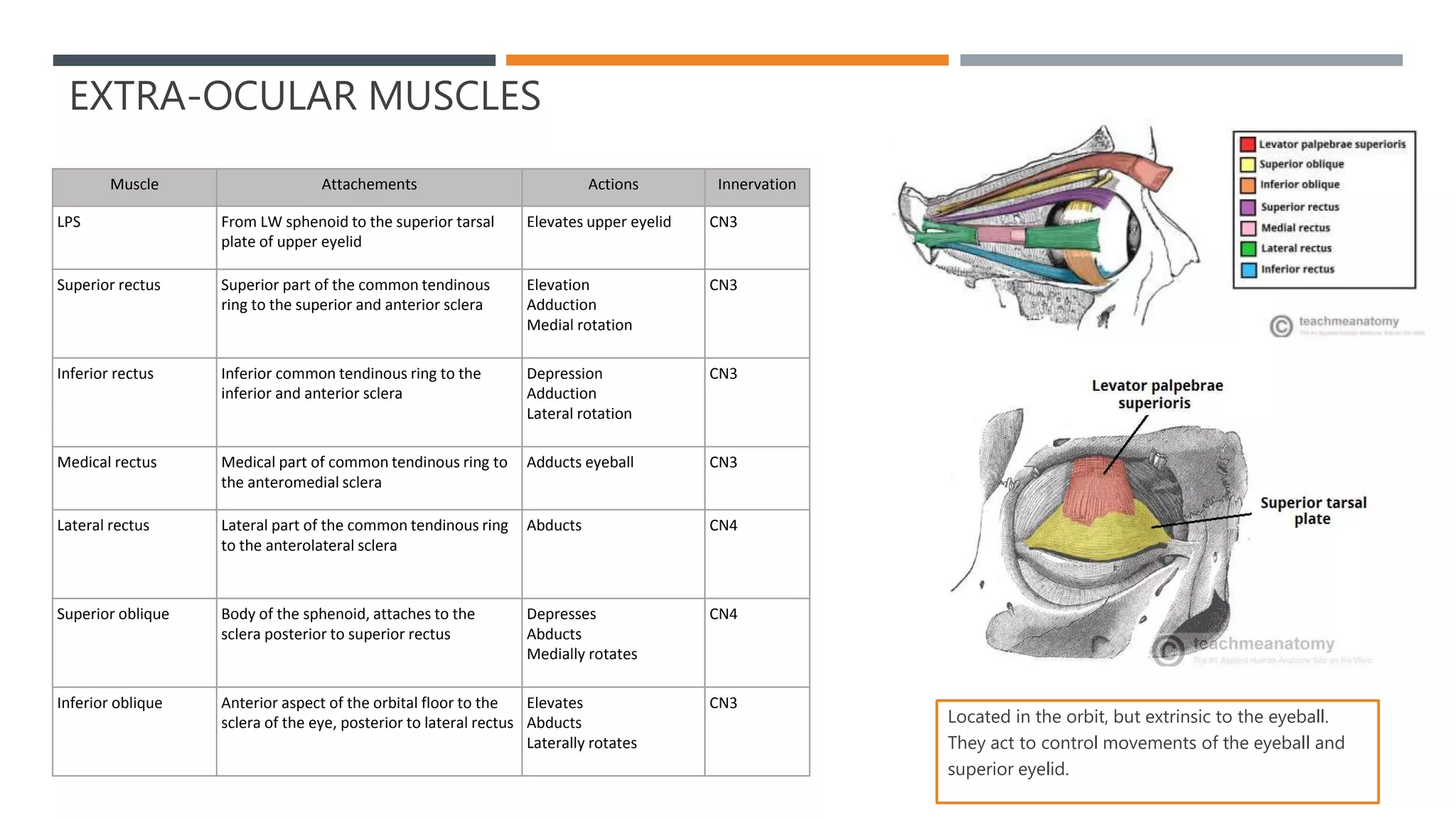
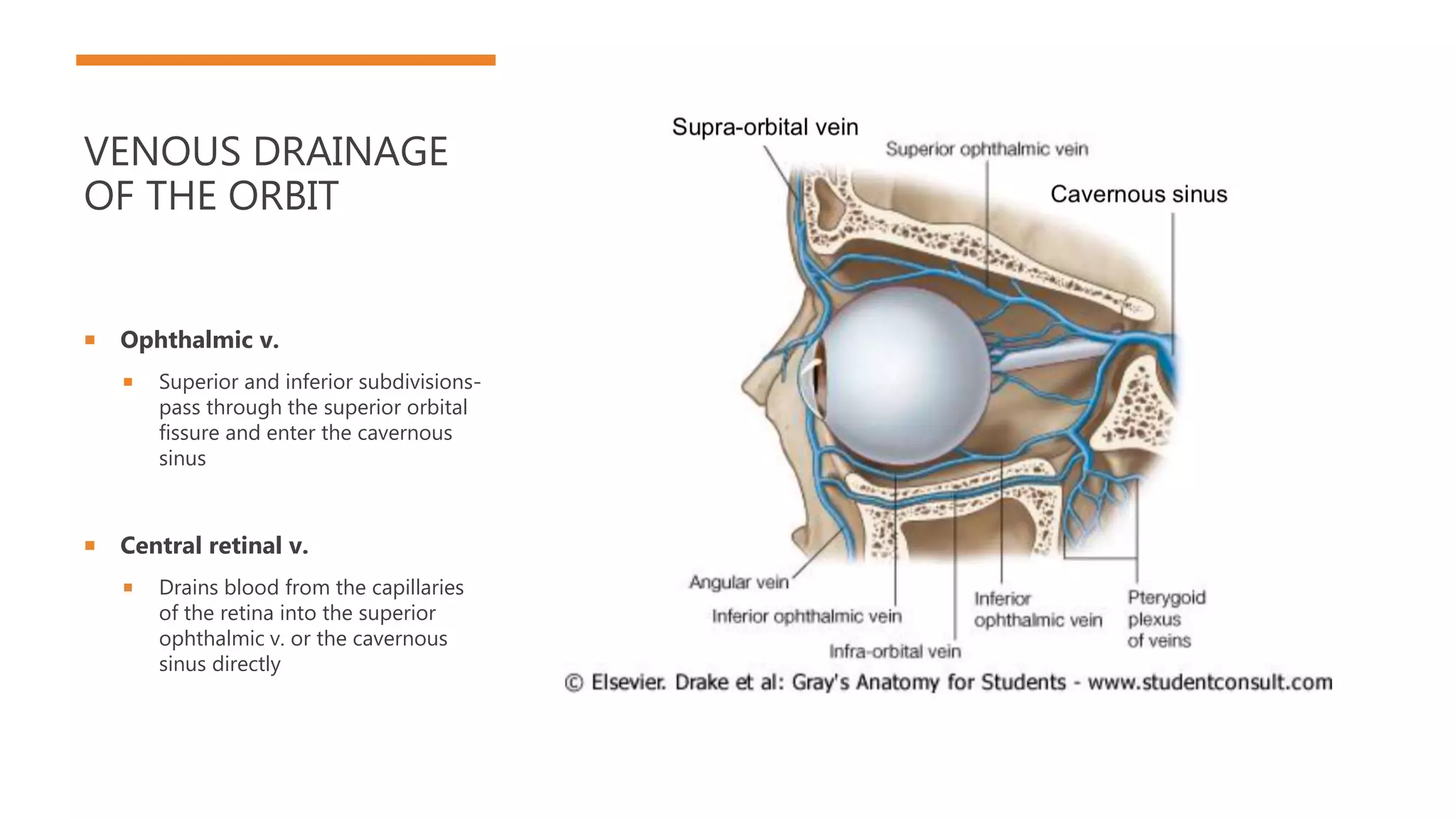
The document describes the anatomy of the eye and orbit. It details the bones that make up the orbit, including the frontal, sphenoid, maxilla, palatine and zygomatic bones. It then discusses the layers of the eyeball, muscles of the eyelid and extraocular muscles. The document outlines the parasympathetic and sympathetic innervation of the eye as well as the blood supply and venous drainage of the orbit.