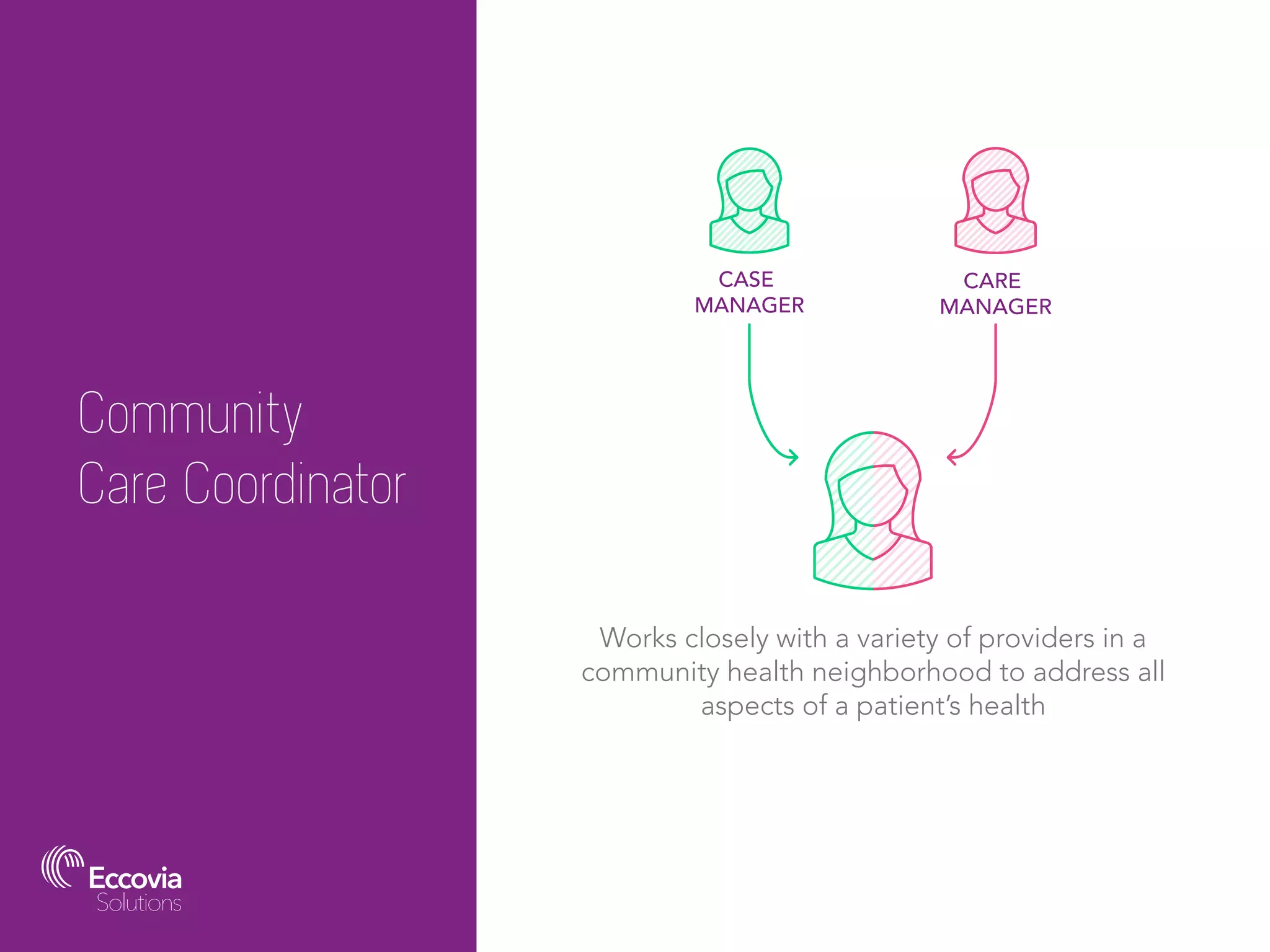
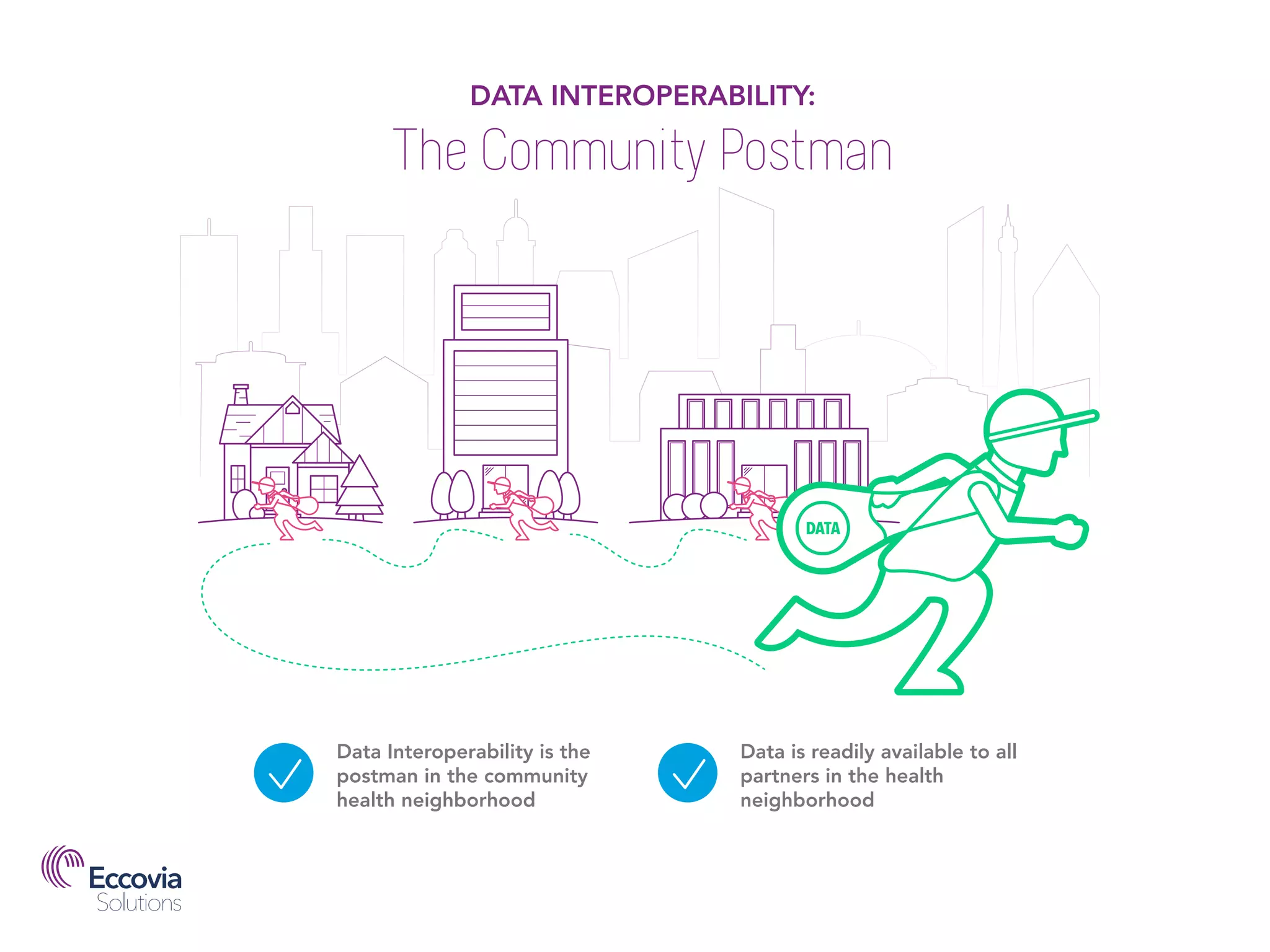
Evolving healthcare delivery models emphasize community care coordination to improve patient outcomes and reduce costs in the US health system. Community care coordinators facilitate collaboration among various providers to address comprehensive patient needs through innovative models like accountable care organizations and patient-centered medical homes. Effective data sharing and interoperability are essential in these networks to support the treatment of individuals with complex health and social issues.