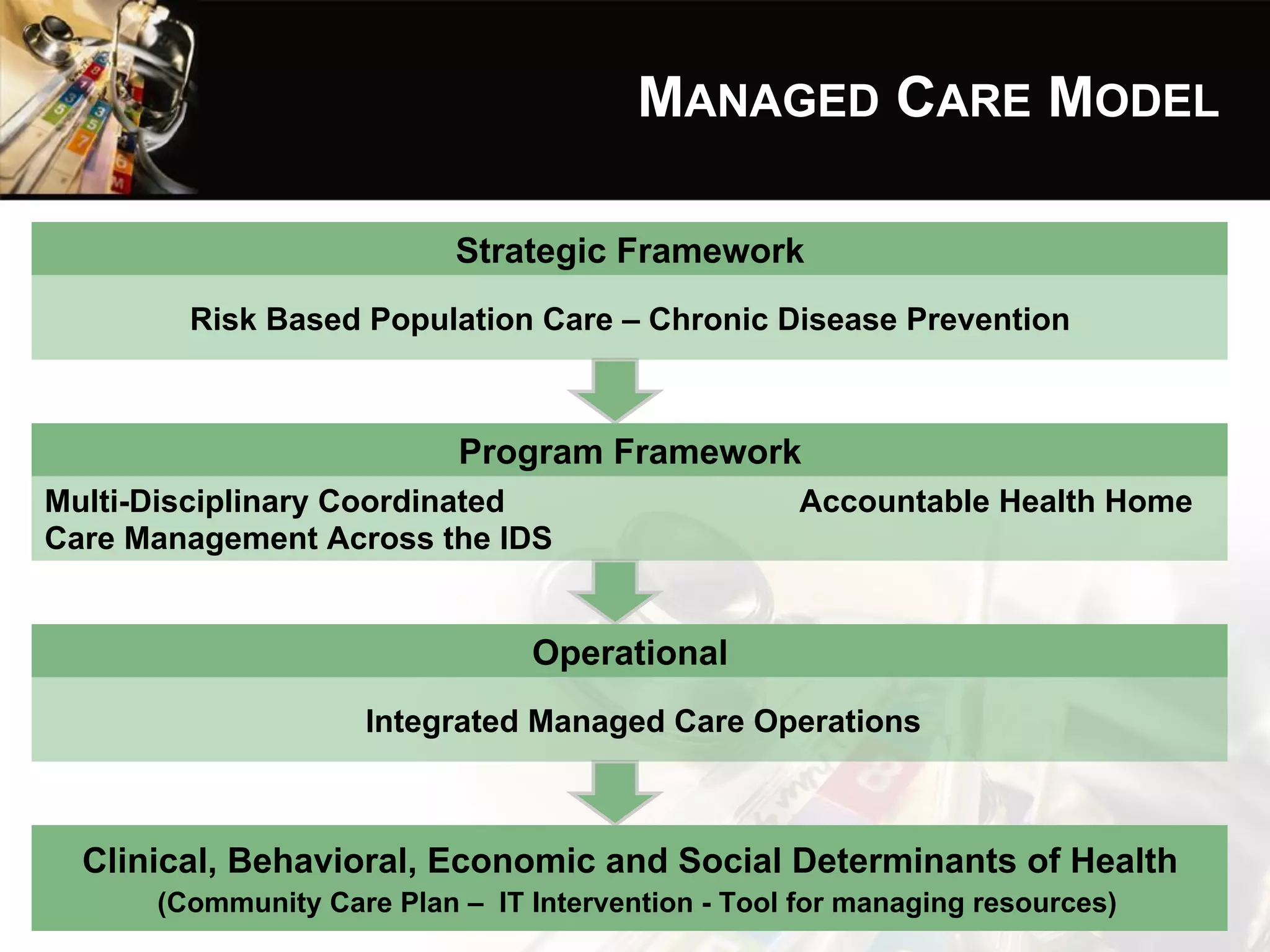
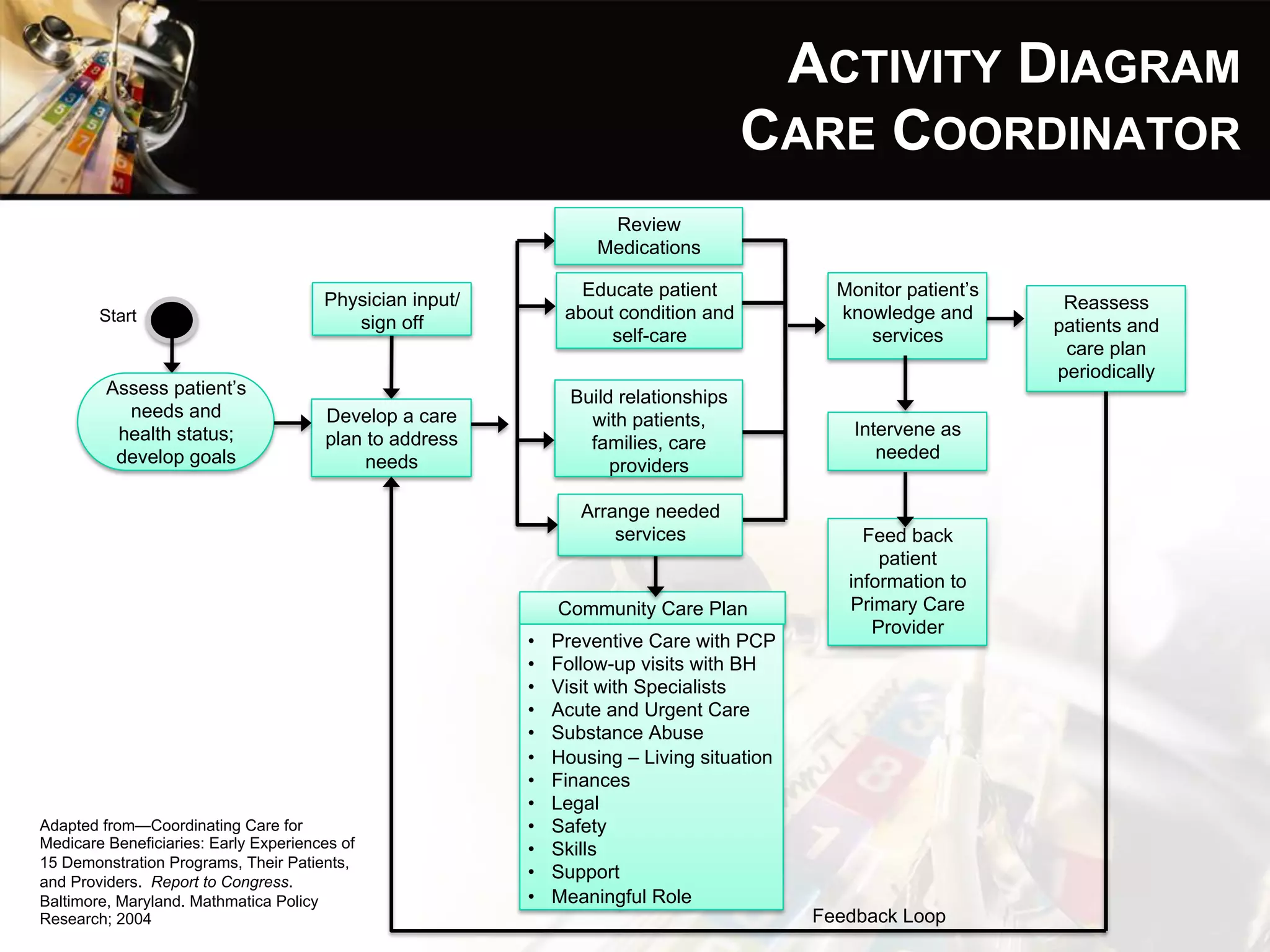
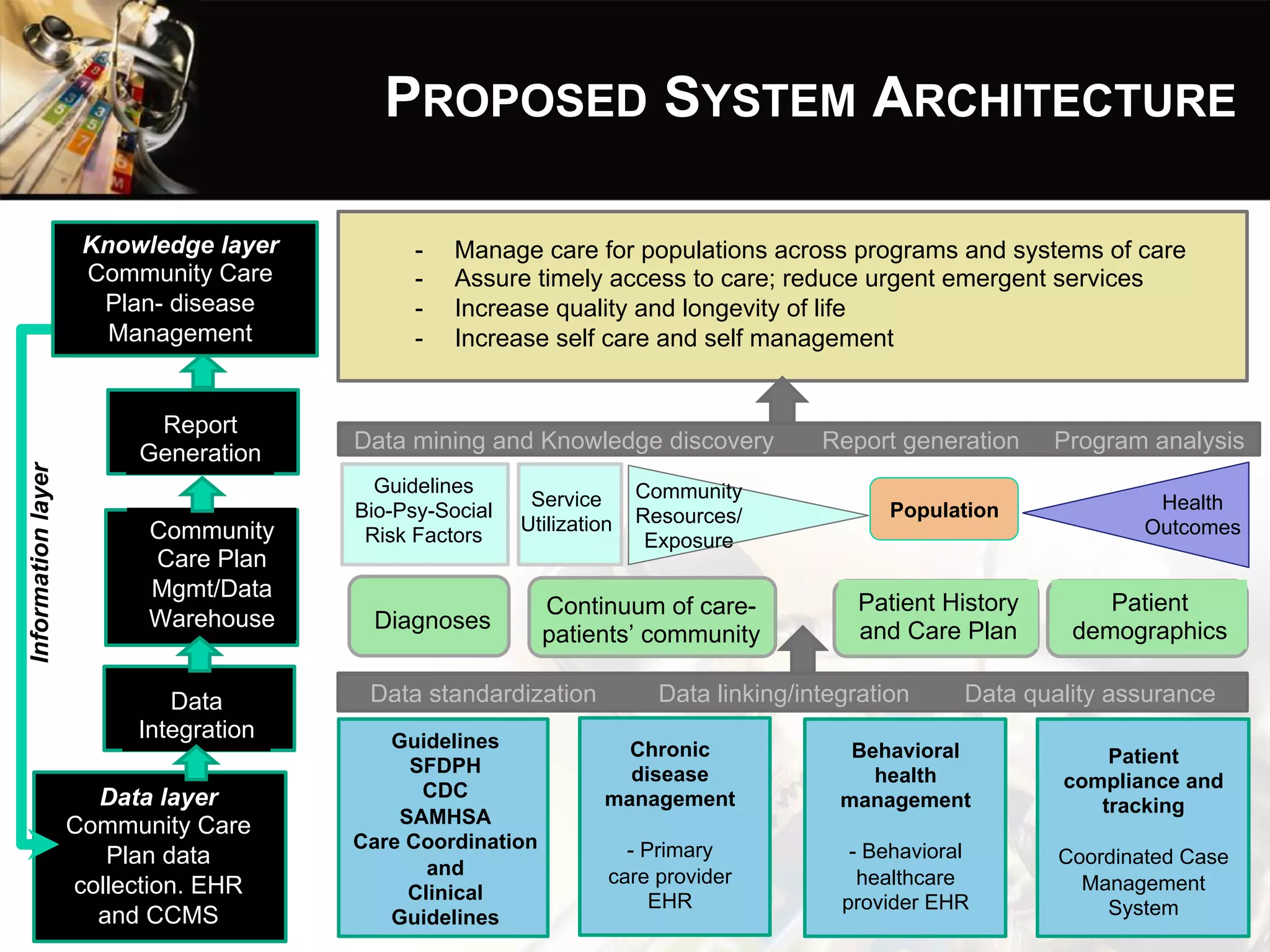
The document outlines a proposed managed care model for the San Francisco Department of Public Health to address social determinants of health through coordinated care management. A multi-disciplinary team would develop community care plans to address patients' clinical, behavioral, economic and social needs. This would be done through an integrated data system and care coordination with providers, social services, and community organizations. The goal is to improve health equity, care quality and access while reducing costs through preventative care management across settings.