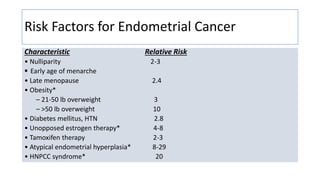
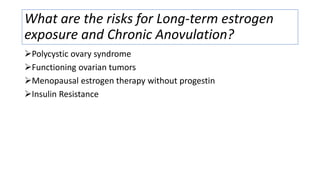
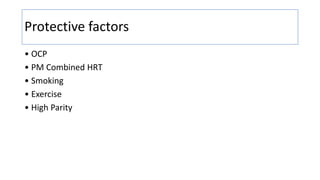
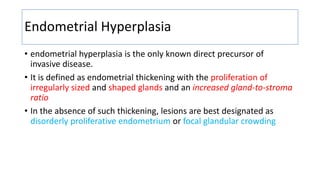
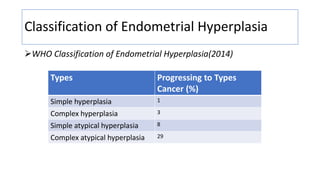
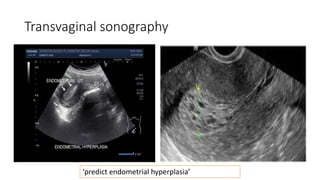
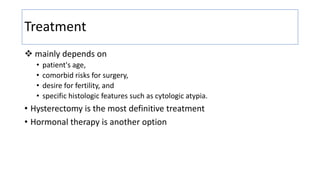
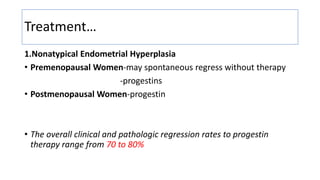
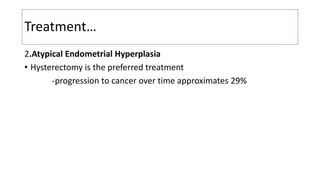
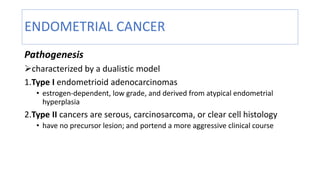
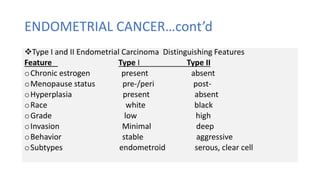
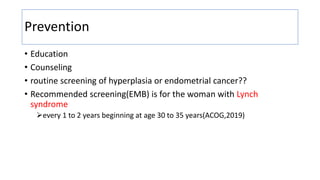
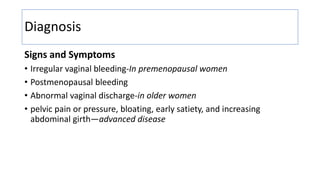
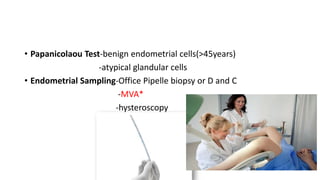
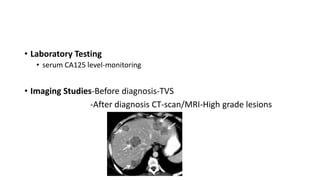
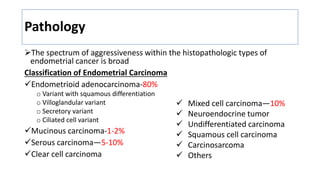
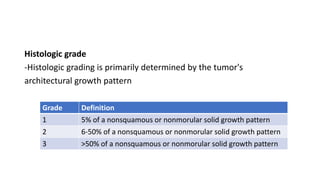
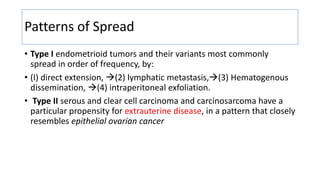
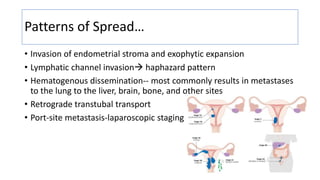
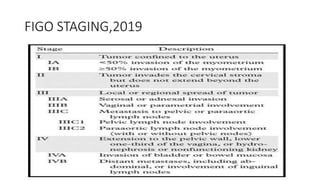
Endometrial cancer is the most common gynecologic malignancy in the U.S. and has rising incidence rates, with key risk factors including obesity and unopposed estrogen therapy. The document outlines classification, clinical features, diagnosis, treatment options, and pathogenesis of endometrial hyperplasia and cancer, emphasizing the importance of histologic evaluation and tailored treatment plans. Preventive measures such as routine screening for high-risk women and education are also highlighted.