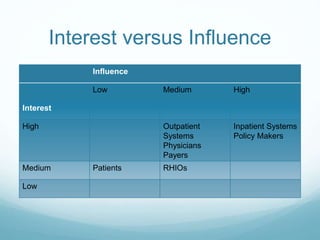
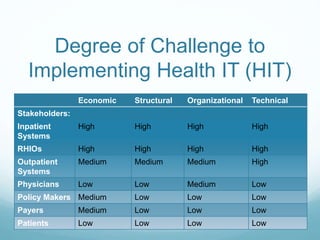
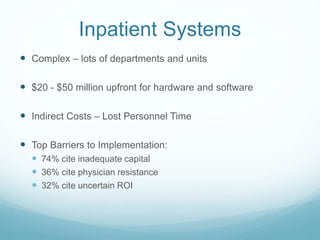
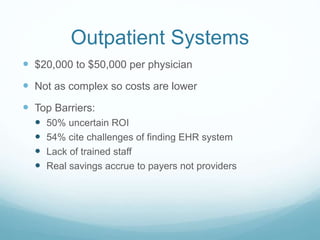
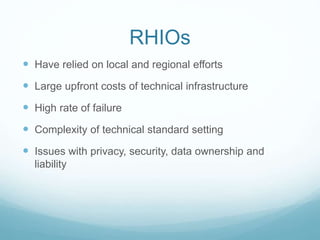
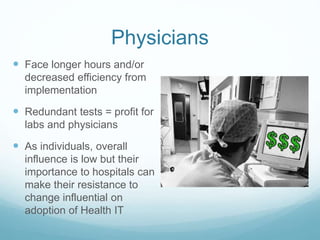
The document discusses the challenges of implementing health information technology (HIT) systems. It identifies four key functionalities of HIT systems and the various stakeholders involved. Inpatient systems face the highest degree of economic, structural, organizational and technical challenges to implementation. Barriers for inpatient systems include inadequate capital, physician resistance, and uncertain return on investment. While outpatient systems, regional health information organizations, and physicians also face challenges, patients, payers and policymakers present the least challenges to implementation and would see the highest savings from HIT.