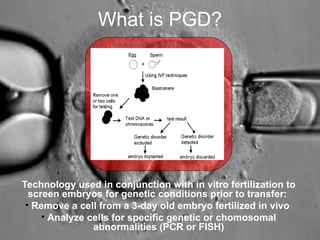
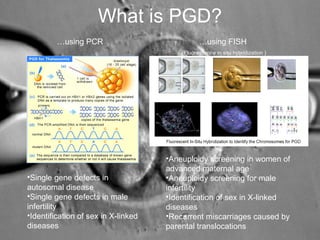
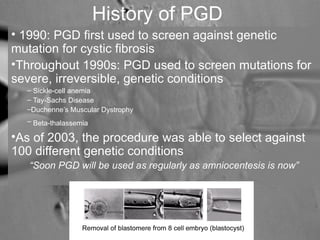
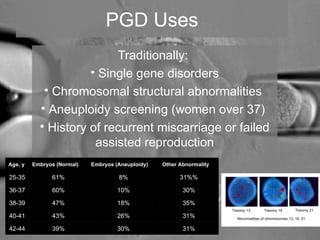
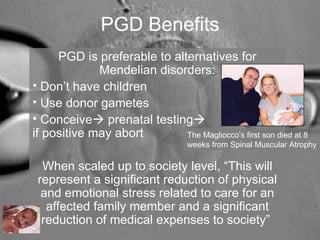
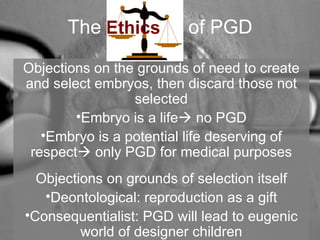
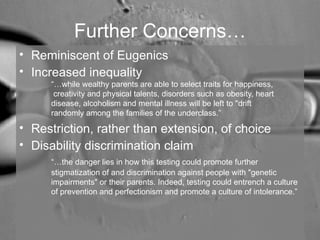
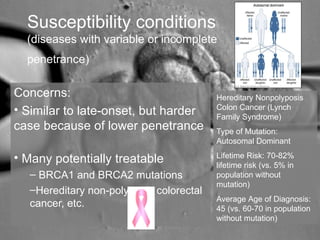
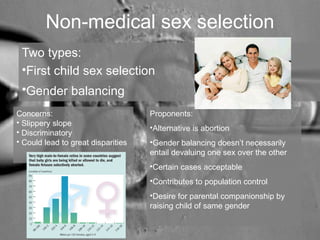
This document discusses the ethical implications of preimplantation genetic diagnosis (PGD), a technology used with in vitro fertilization to screen embryos for genetic conditions prior to implantation. It outlines how PGD has been used to screen for single-gene disorders, chromosomal abnormalities, and susceptibility genes. While PGD can prevent transmission of genetic diseases, its use raises ethical concerns such as eugenics, inequality, and disability discrimination. The document examines debates around using PGD for late-onset conditions, tissue typing to save a sibling's life, non-medical sex selection, and selection for non-medical traits. Determining where to draw the line on its applications remains challenging.