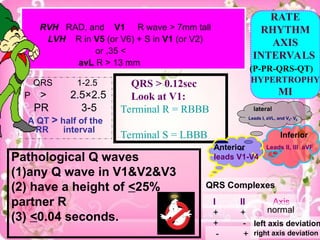
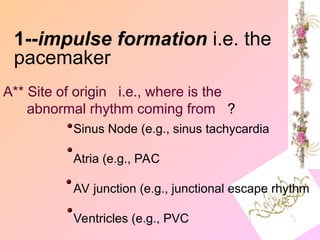
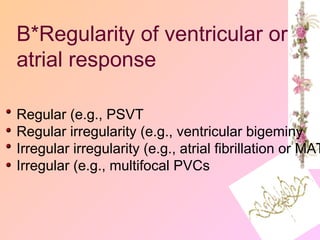
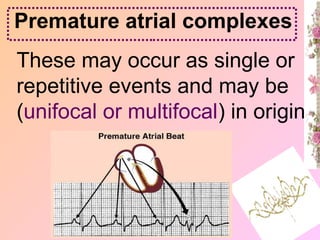
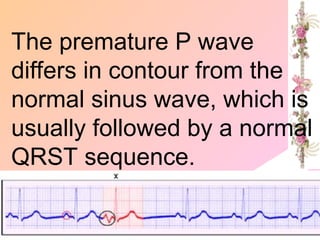
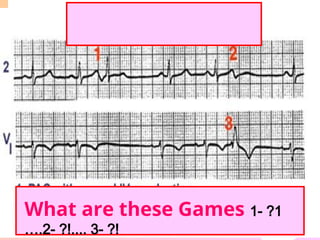
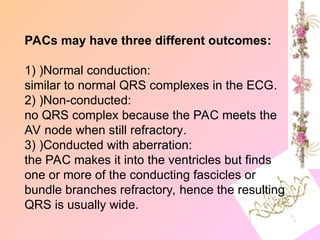
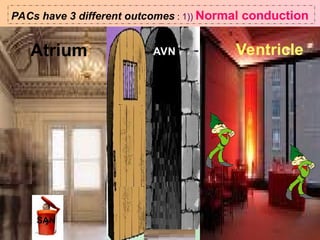
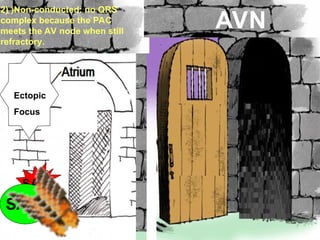
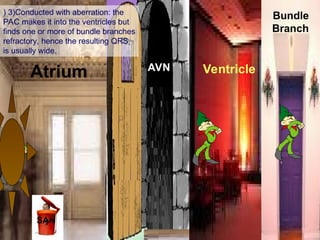
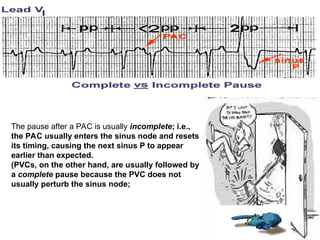
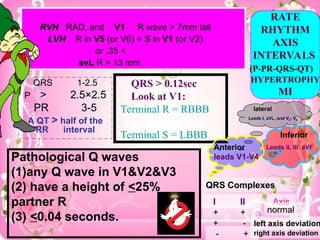
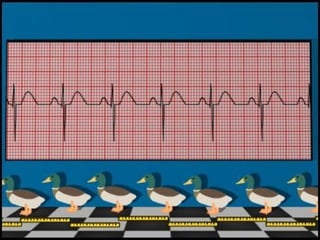
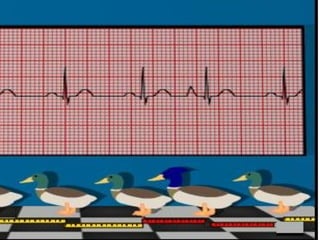
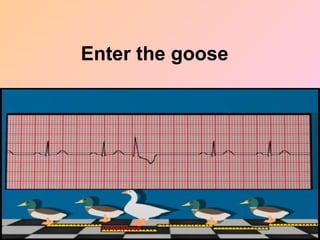
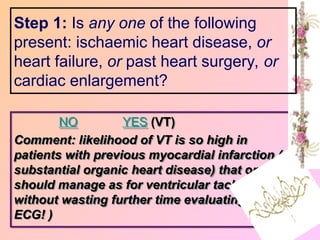
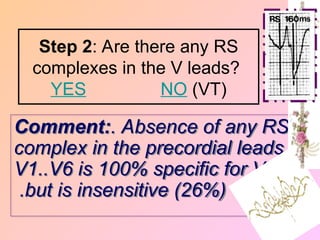
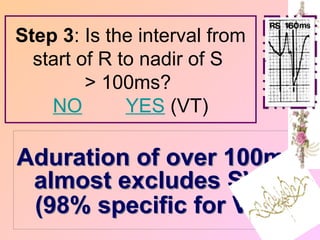
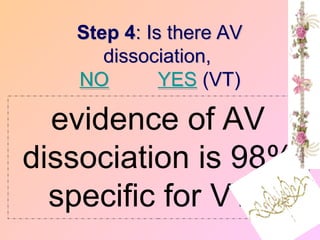
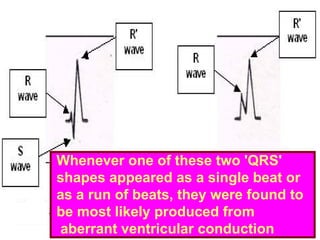
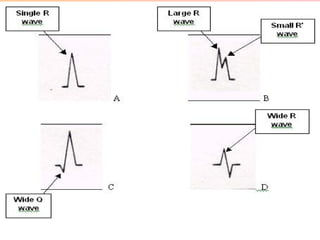
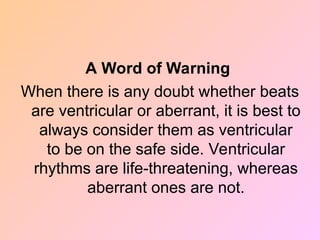
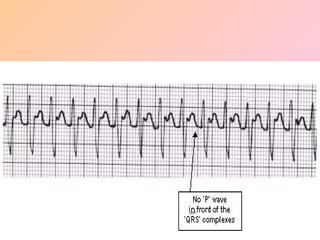
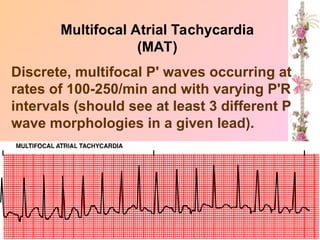
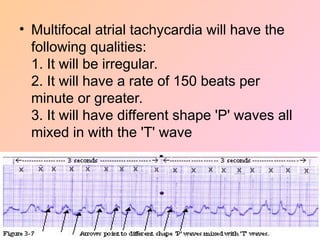
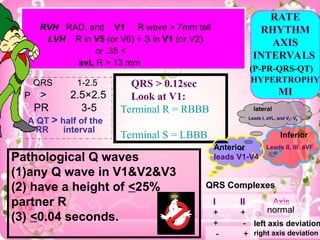
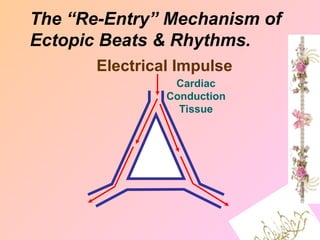
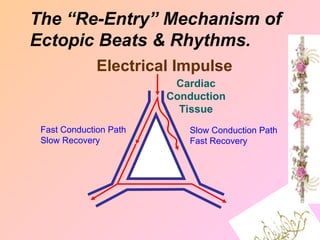
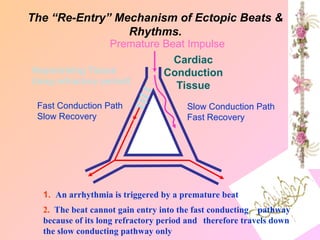
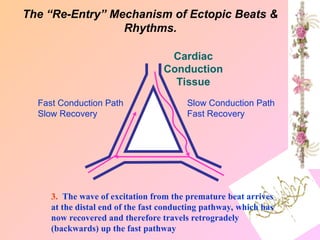
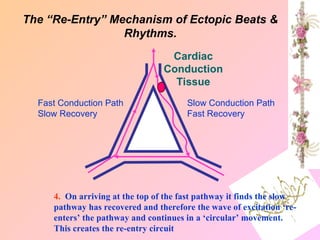
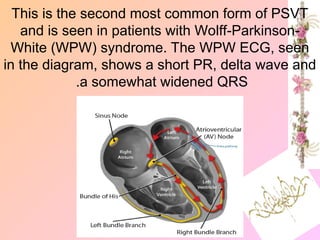
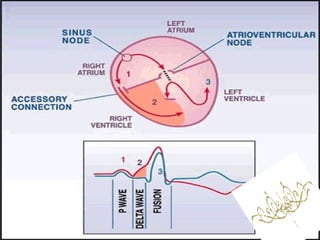
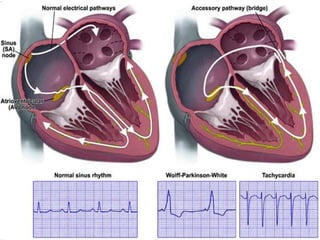
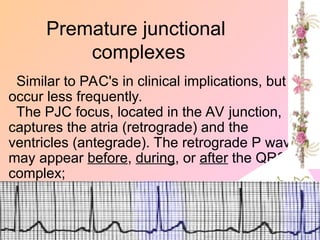
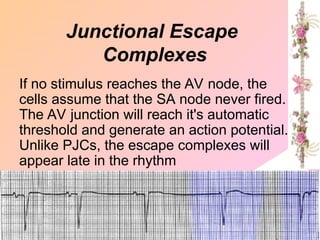
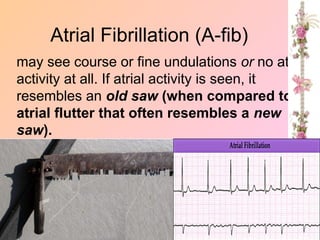
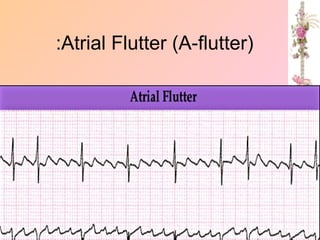
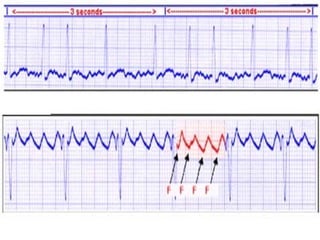
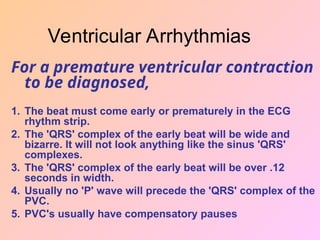
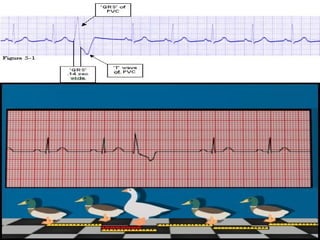
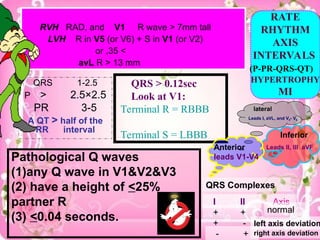
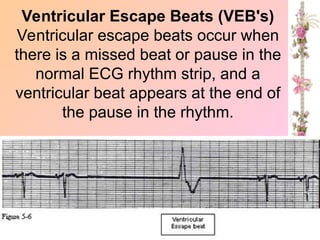
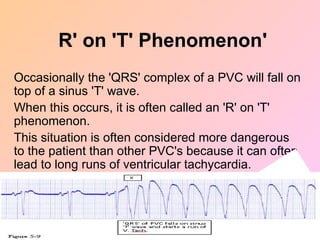
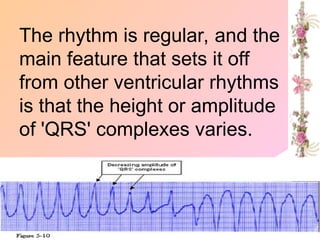
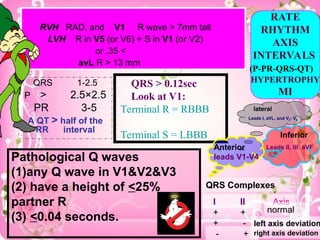
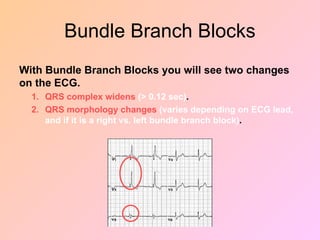
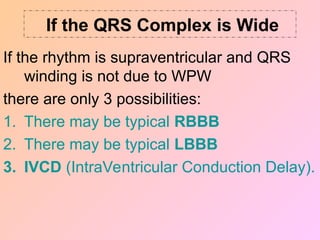
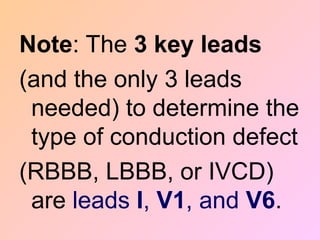
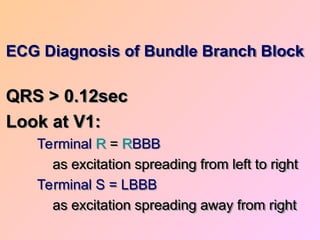
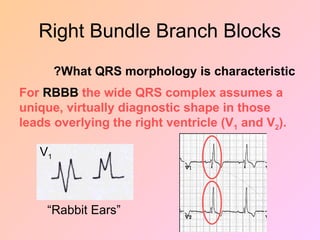
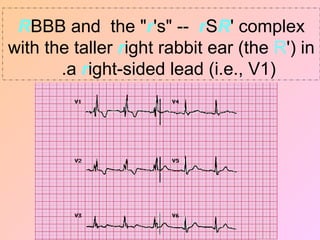
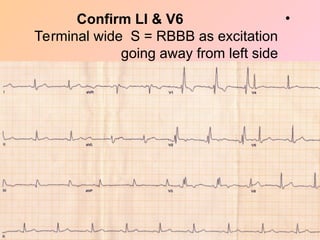
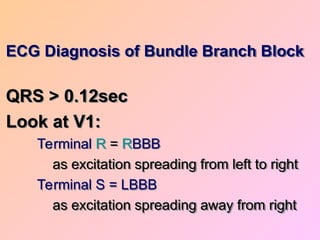
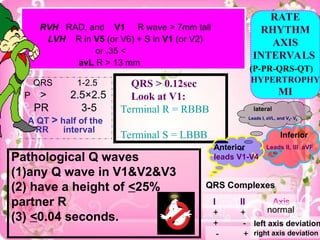
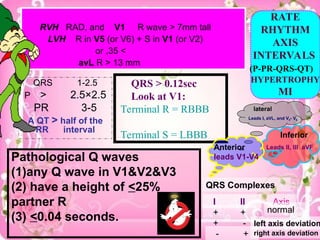
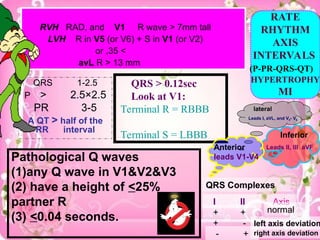
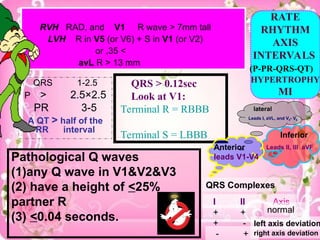
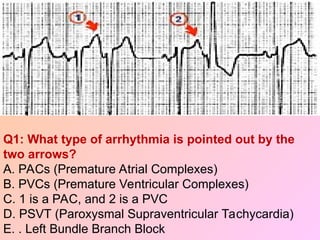
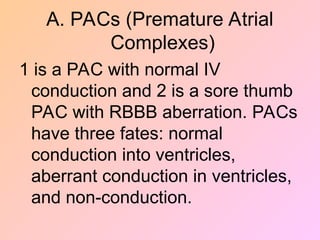
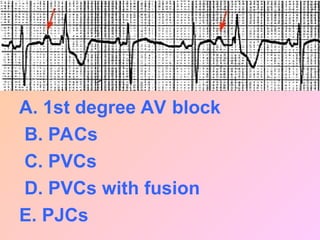
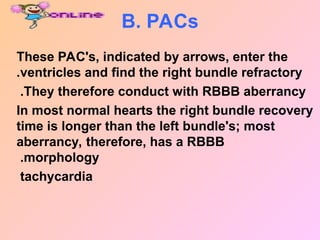
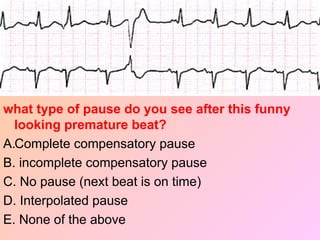
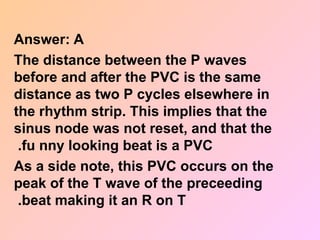
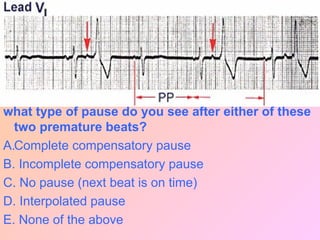
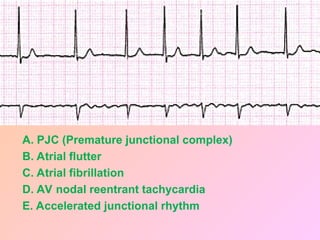
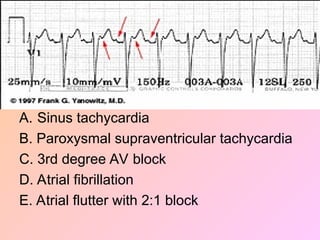
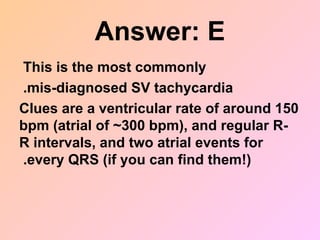
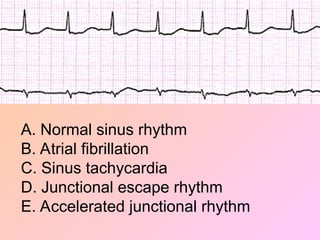
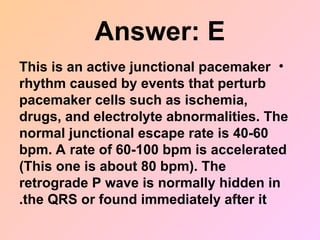
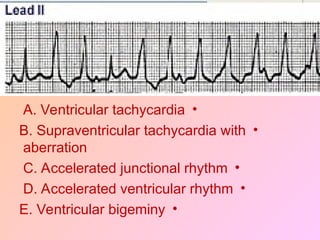
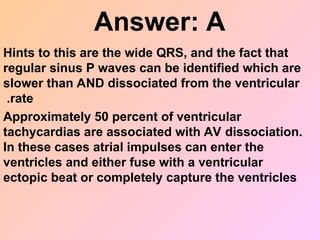
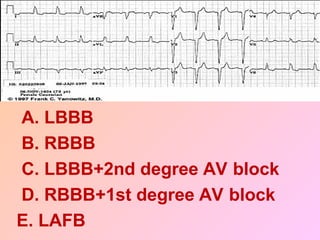
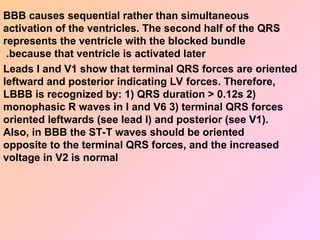
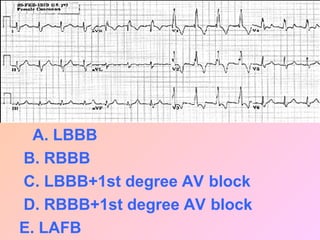
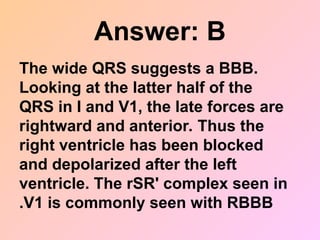
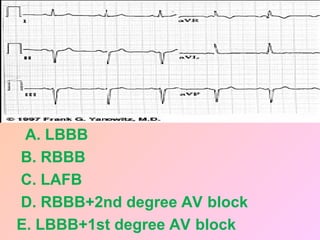
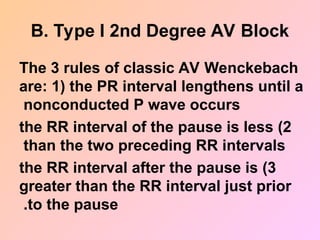
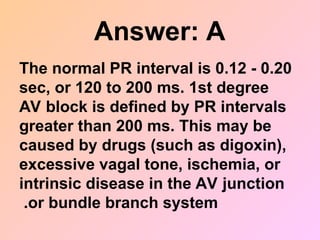
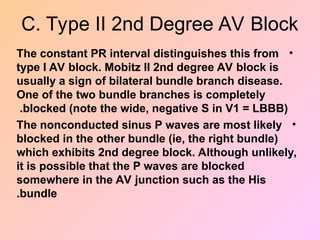
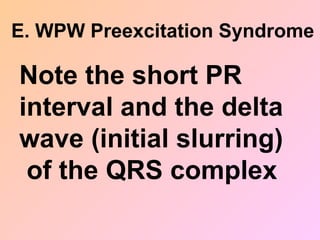
The document provides an extensive overview of various cardiac arrhythmias, including their characteristics, diagnosis, and implications for treatment. It details how to identify different types of arrhythmias like premature atrial complexes, supraventricular tachycardia, and ventricular tachycardia, emphasizing the importance of specific ECG features. Additionally, it discusses mechanisms of impulse formation and conduction, as well as treatment options for these arrhythmias.