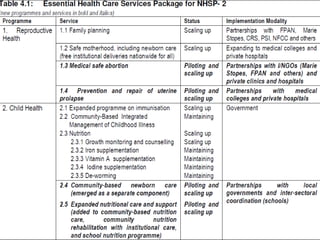
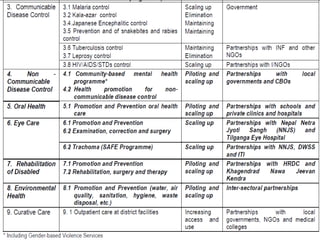
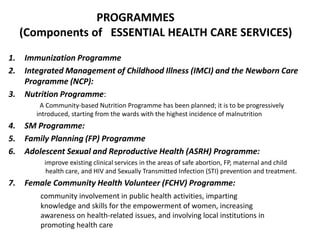
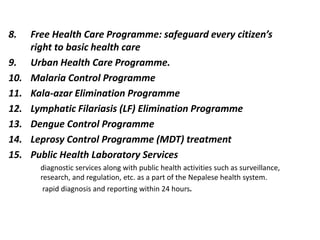
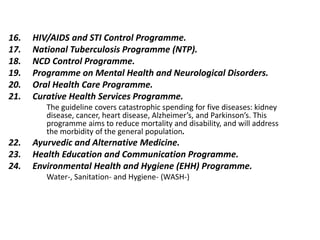
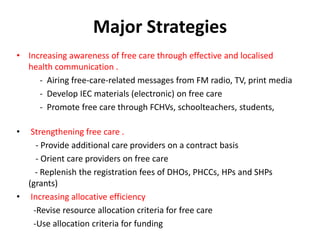
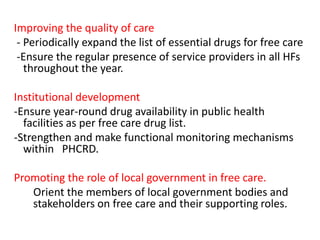
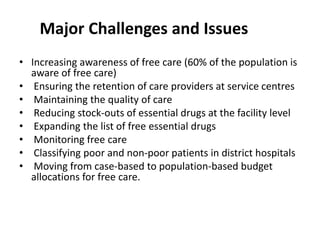
This document summarizes Nepal's Essential Health Care Services and Free Health Care Programme. It defines Essential Health Care Services as basic health services provided equitably and cost-effectively by the government. The government aims to increase access to EHCS, especially for women, the poor, and rural populations. The Free Health Care Programme was created to safeguard citizens' right to basic care by making EHCS free of charge at many facilities. The program goals are to reduce health costs for vulnerable groups and address morbidity. It faces challenges in awareness, provider retention, quality, drug stockouts, and monitoring.