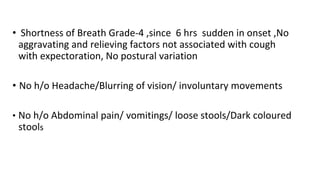
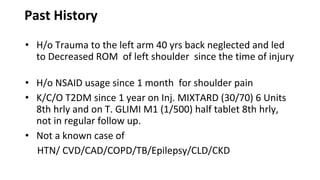
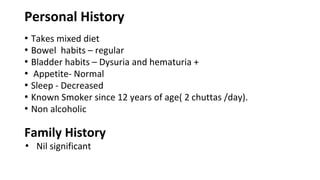
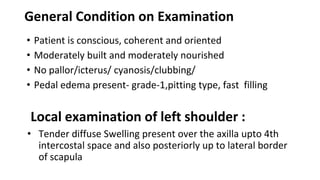
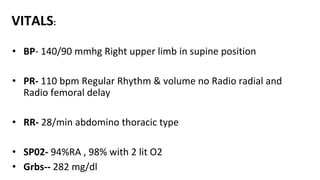
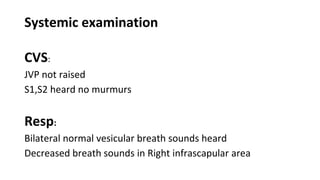
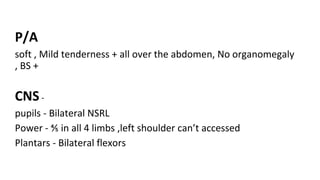
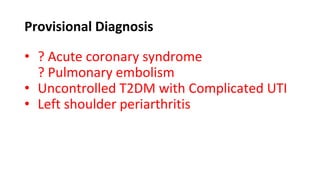
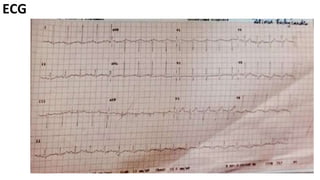
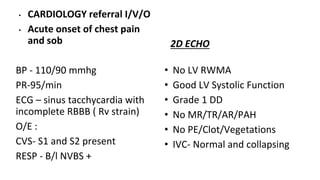
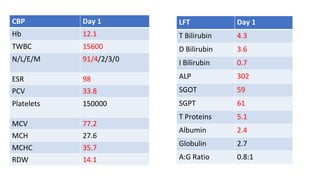
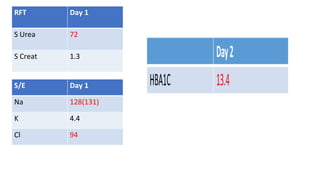
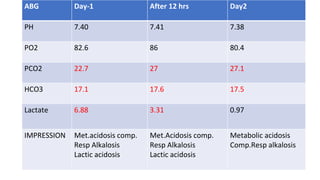
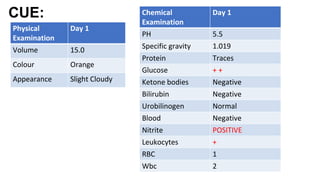
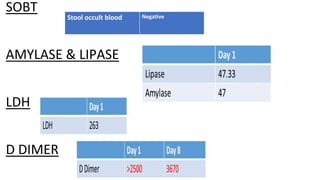
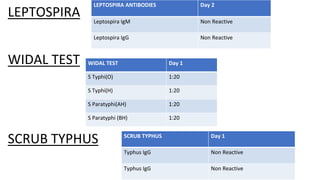
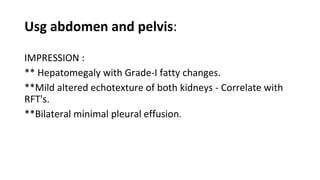
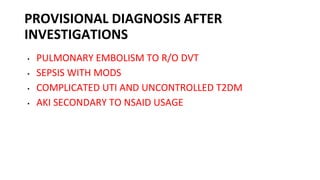
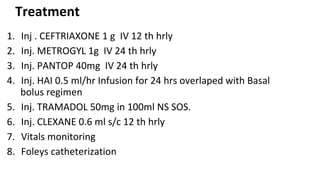
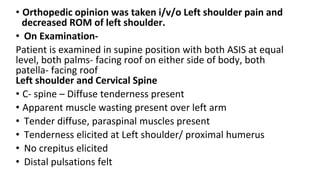
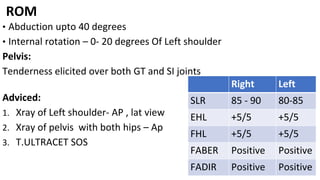
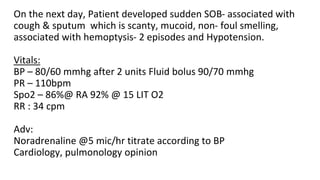
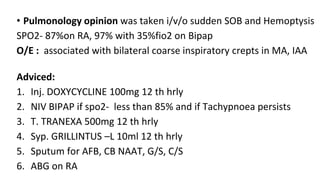
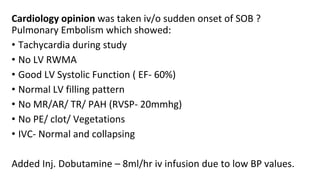
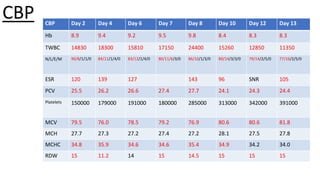
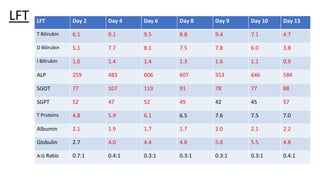
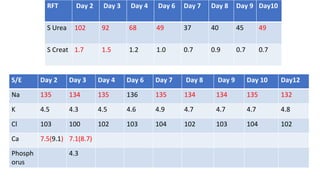
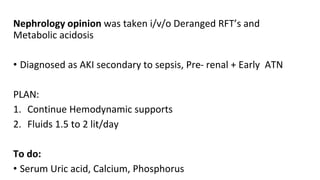
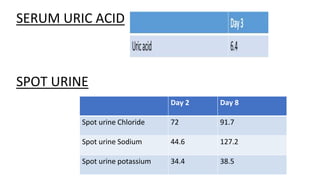
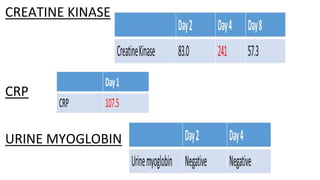
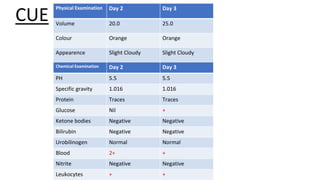
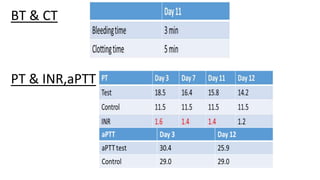
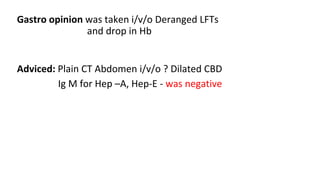
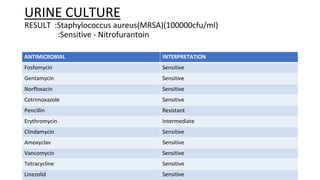
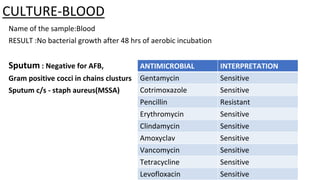
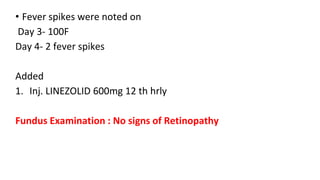
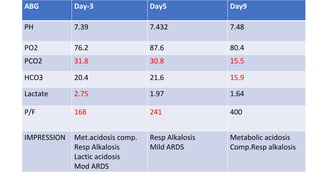
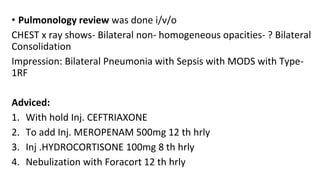
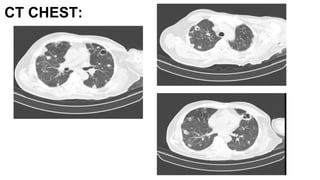
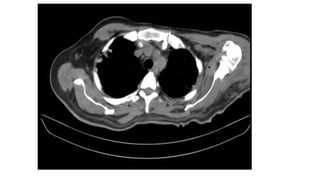
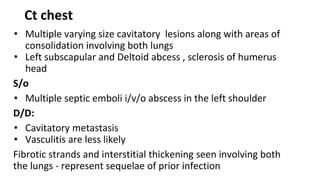
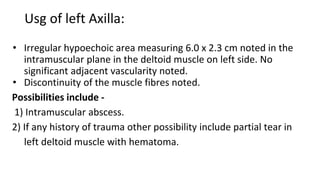
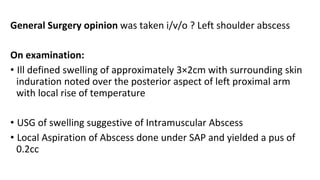
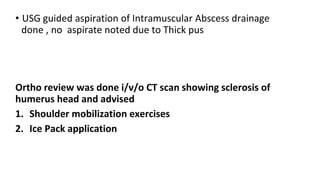
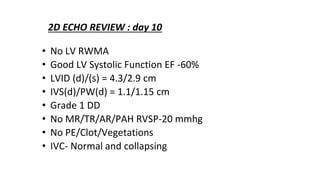
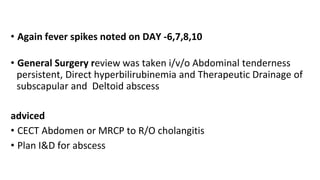
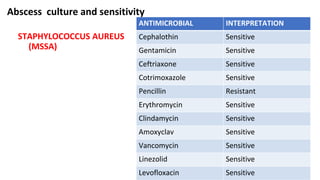
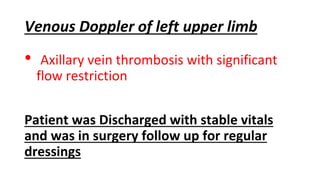
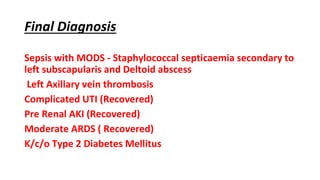
A 60-year-old male presented with multiple symptoms including shoulder pain, fever, chest pain, shortness of breath, and hematuria, alongside a history of uncontrolled diabetes and past shoulder trauma. Diagnostic workup suggested pulmonary embolism, complicated urinary tract infection, sepsis, and acute kidney injury. The patient received extensive medical treatment including antibiotics, steroids, and continuous monitoring in response to evolving clinical conditions and complications.