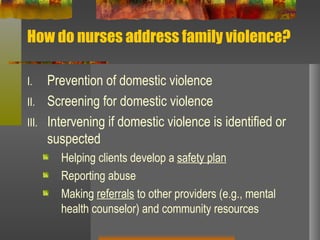
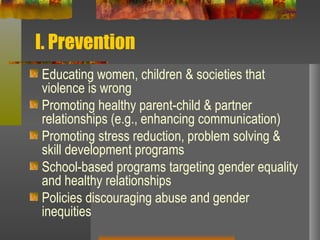
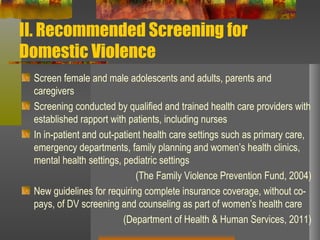
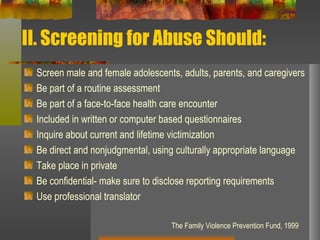
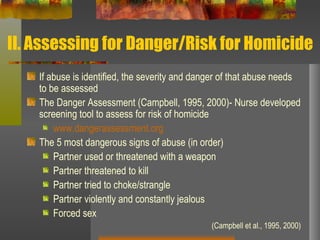
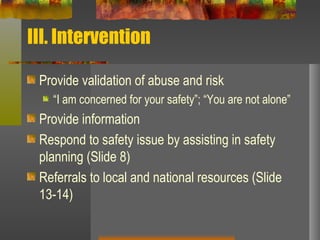
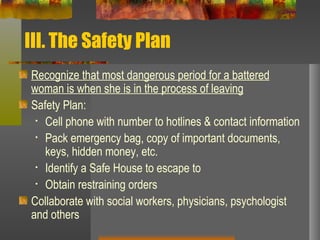
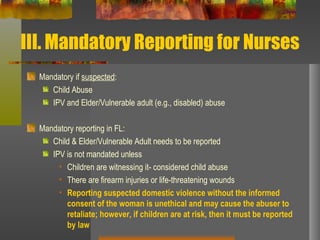
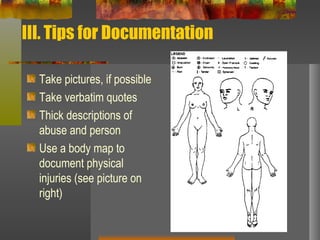
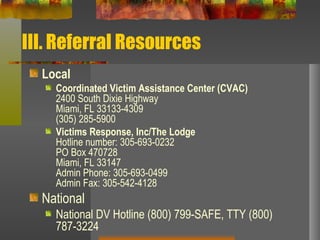
This document outlines the roles and responsibilities of nurses in addressing domestic violence. It discusses prevention through education, screening patients for abuse, assessing level of danger if abuse is identified, developing safety plans, mandatory reporting requirements, documentation, and providing referrals to local and national support resources. The goals are to identify those experiencing abuse, ensure their safety, and connect them with services and support.
![Unit 4: Roles and Responsibilities of Nurses in Addressing Domestic Violence Rosa Maria Gonzalez-Guarda, PhD, MPH, RN, CPH Assistant Professor School of Nursing & Health Studies University of Miami [email_address]](https://image.slidesharecdn.com/dvtrainingunit410-18-11-111031094827-phpapp02/85/Dv-training-unit-4-10-18-11-1-320.jpg)