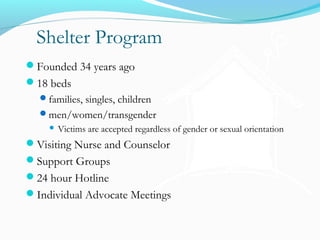
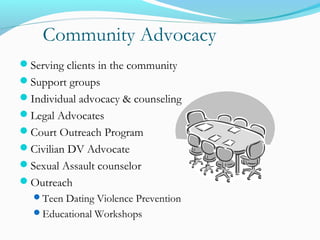
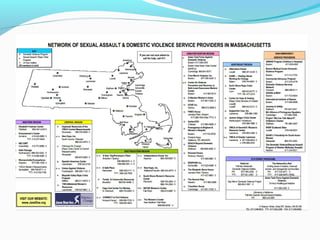
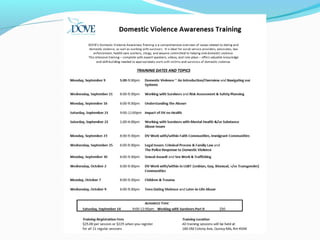
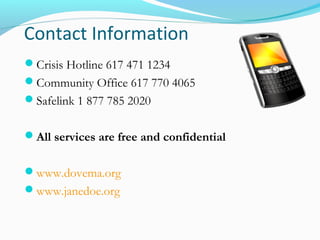
DOVE, Inc provides shelter, advocacy, and support services to victims of domestic violence. It operates an 18-bed shelter that accepts families, individuals, children, and people of all genders and orientations. It also offers community advocacy programs, legal assistance, counseling, and educational workshops. The organization works to promote safety and empower victims by addressing the complex health, social, and legal impacts of domestic violence.