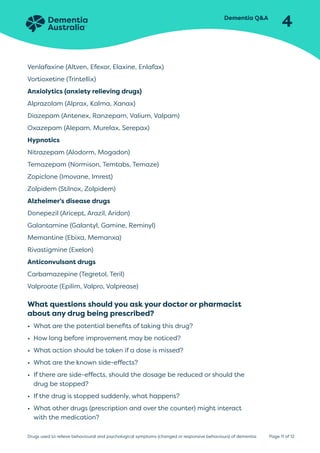
People with dementia may develop behavioral and psychological symptoms like depression, anxiety, or aggression. While non-drug interventions should be tried first, medication may sometimes be necessary, though drugs have side effects. Antipsychotics are commonly used but have risks and limited benefits, and should generally only be used for up to three months. Other options include anticonvulsants or antidepressants, which require specialist prescription. All drug treatment for dementia symptoms requires careful monitoring and review.