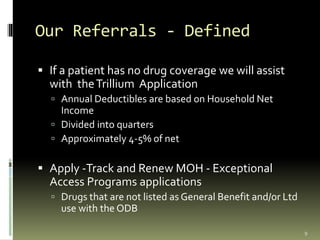
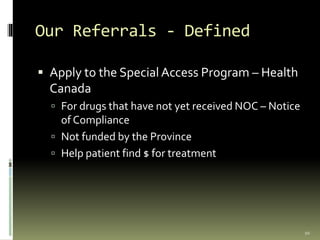
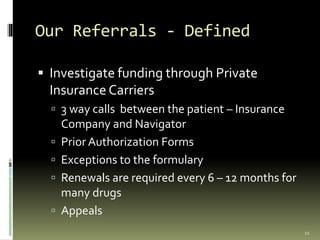
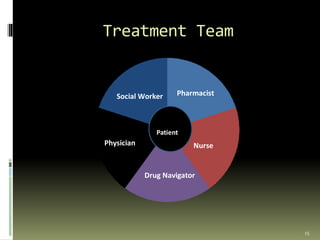
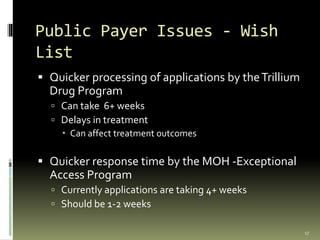
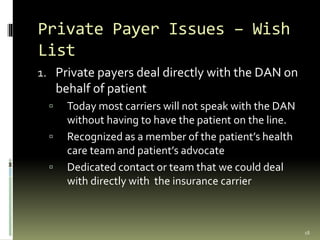
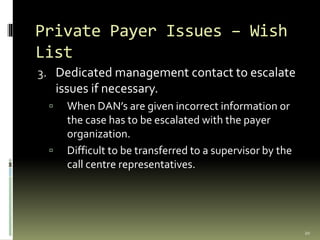
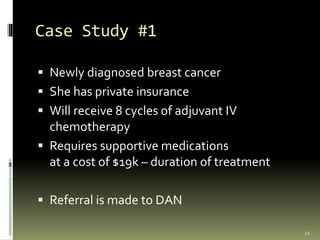
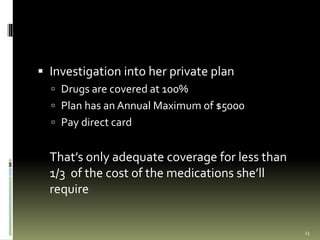
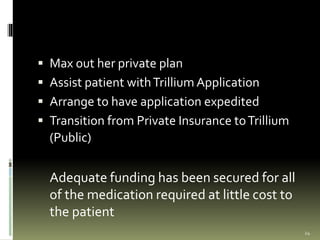
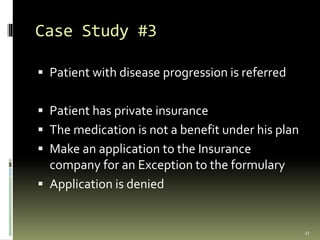
ODANO (Oncology Drug Access Navigators of Ontario) is a provincial organization that provides support and advocacy to help cancer patients access the medications they need. It has over 50 members across various regions of Ontario who help navigate public and private drug coverage plans and work with patients' treatment teams. The organization faces challenges with wait times for public drug plans and lack of direct communication with private insurers, and works on case studies to help patients receive adequate funding for their cancer treatments.