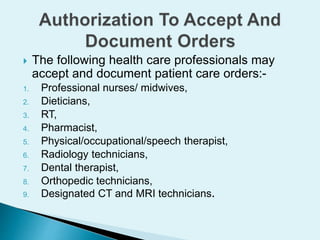
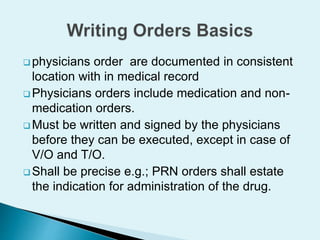
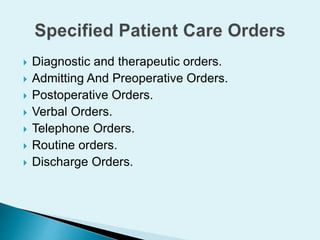
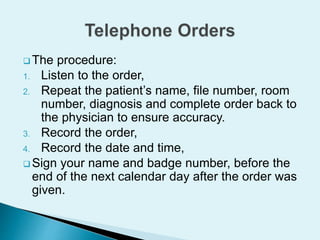
The document establishes guidelines for proper documentation in medical records to ensure effective communication between healthcare professionals and compliance with legal responsibilities, noting that orders must be clear, concise, organized, legible, and evaluated regularly for changes in patient condition. It outlines the roles and responsibilities of various professionals who can accept and document patient care orders, and provides standards for ensuring orders are appropriate, reasonable, and promptly questioned if issues arise.