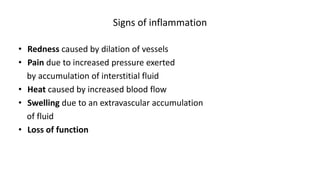
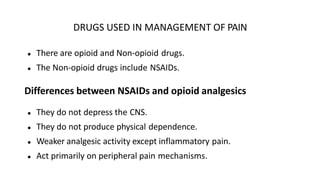
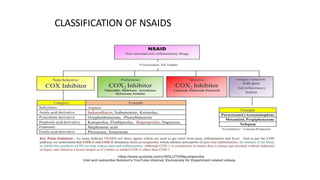
The document discusses drugs used for pain and inflammation management. It begins by defining inflammation, analgesics, NSAIDs, and antipyretics. NSAIDs like aspirin, ibuprofen, and paracetamol are described in more detail, including their mechanisms of action, pharmacokinetics, therapeutic uses, and adverse effects. Specific concerns for NSAID use in pregnancy and risks of overdose like Reye's syndrome and hepatitis are also summarized. The document provides an overview of pharmacotherapy options for pain and fever treatment.