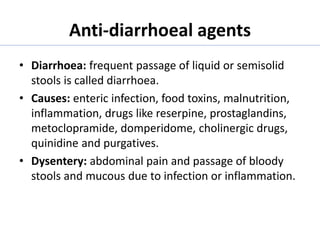
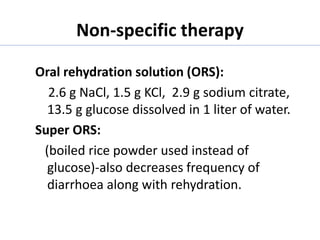
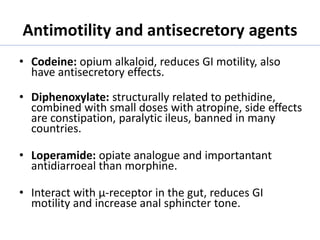
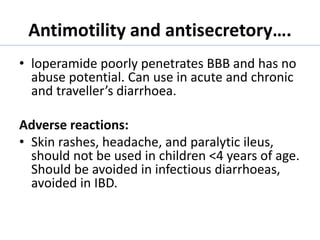
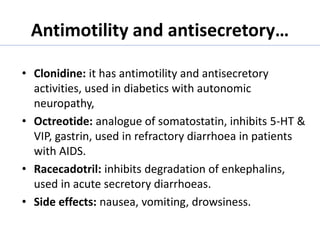
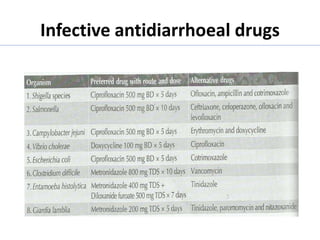
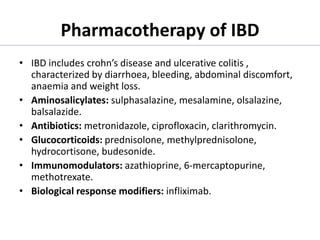
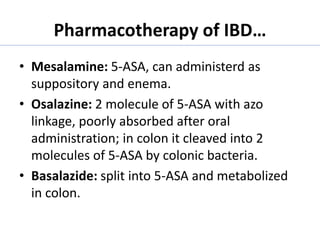
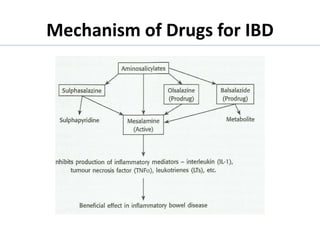
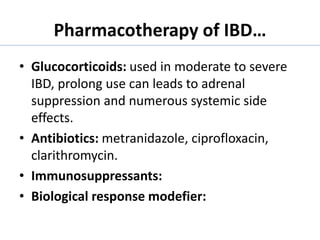
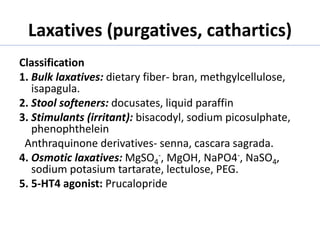
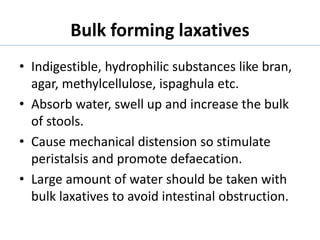
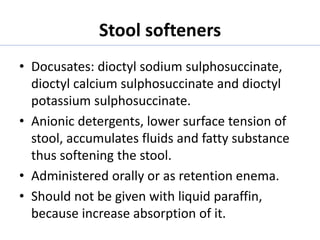
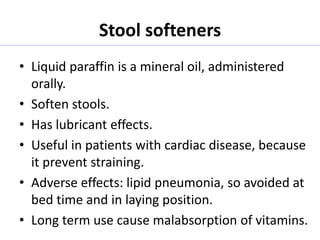
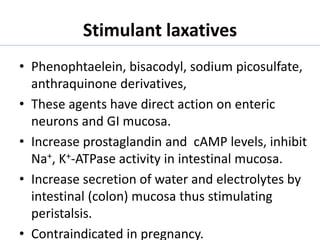
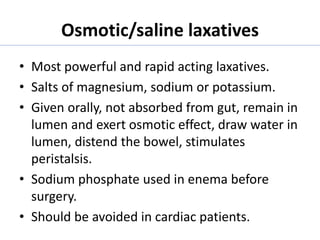
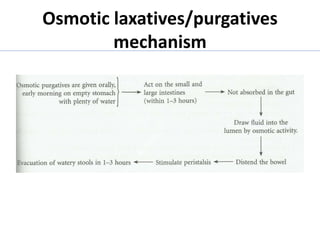
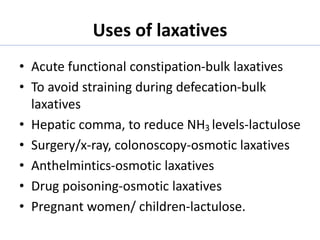
This document discusses drugs used to treat diarrhea and constipation. It describes various causes of diarrhea and different types of laxatives. Oral rehydration solutions and antimotility drugs like loperamide, clonidine and octreotide are used to treat diarrhea. Bulk-forming, stool softening, and stimulant laxatives are described for treating constipation. Drugs used for inflammatory bowel disease like 5-aminosalicylates, corticosteroids, antibiotics, and biologics are also summarized.