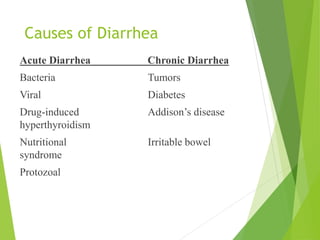
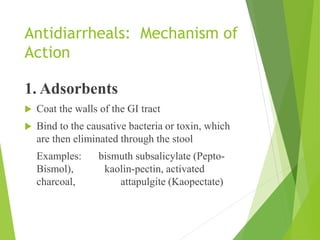
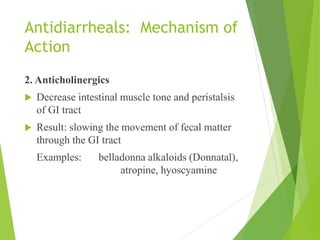
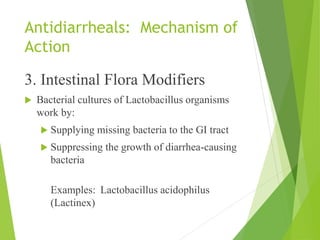
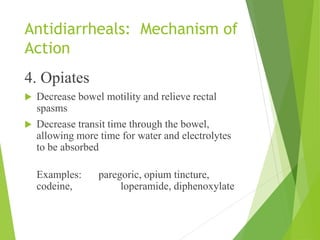
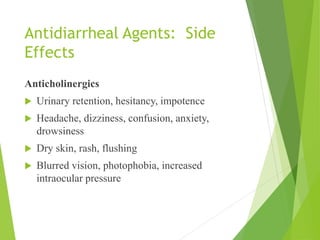
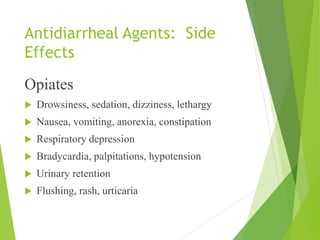
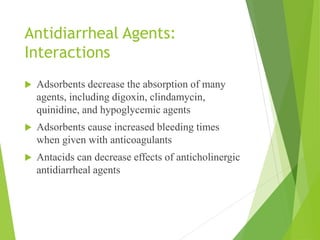
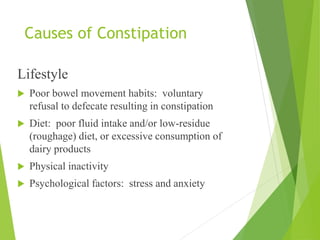
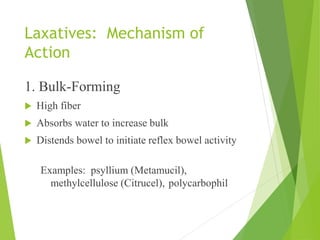
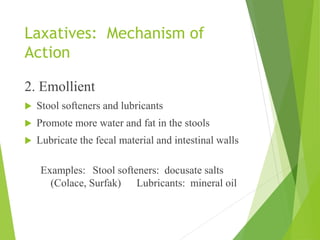
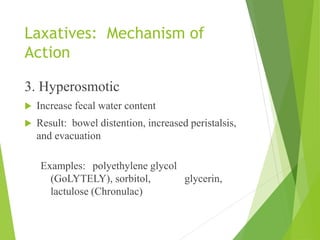
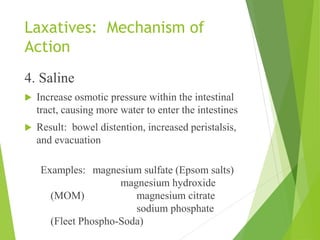
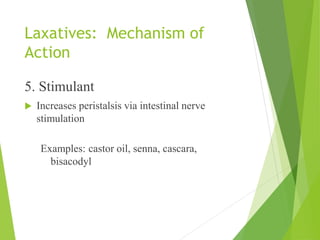
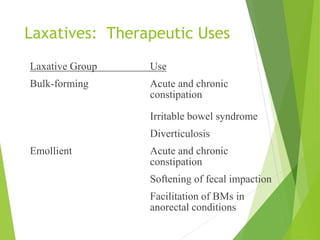
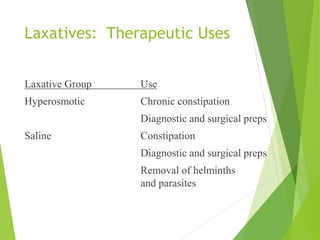
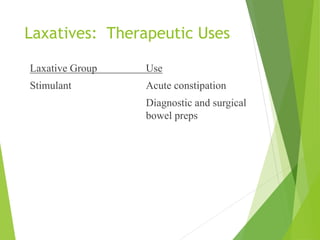
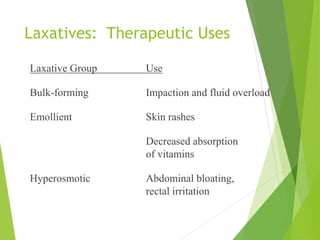
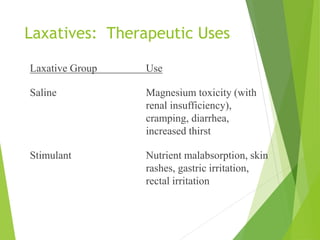
This document discusses drugs that affect the gastrointestinal system, focusing on antidiarrheals and laxatives. It defines diarrhea and constipation and outlines causes of each. It describes the mechanisms of action of various antidiarrheal and laxative agents including adsorbents, anticholinergics, opiates, bulk formers, emollients, hyperosmotics, salines, and stimulants. It notes therapeutic uses and side effects to consider for each drug class. Nursing implications are provided around assessment, education, monitoring, and addressing side effects and interactions.