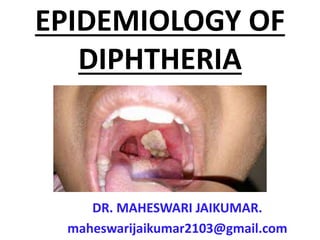
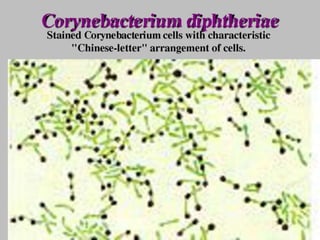
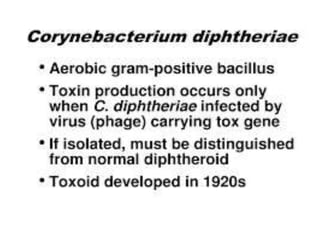
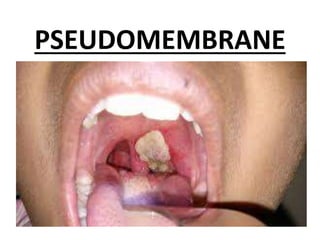
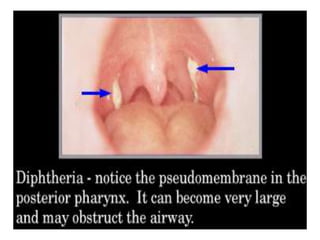
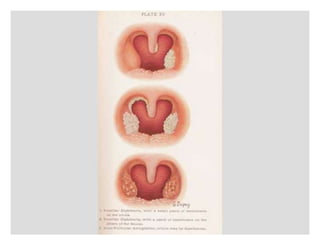
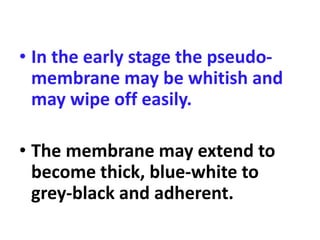
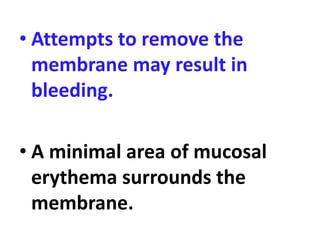
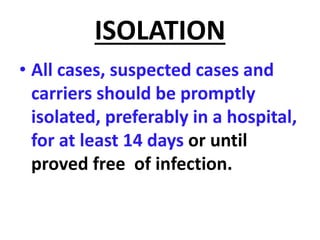
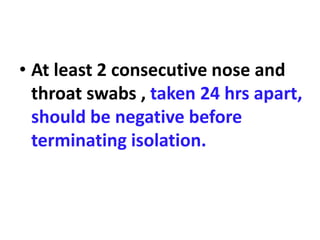
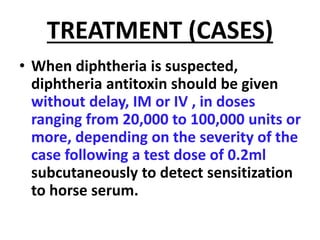
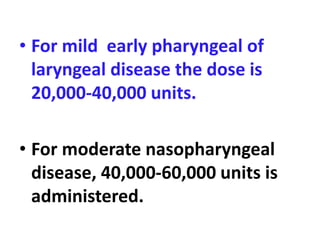
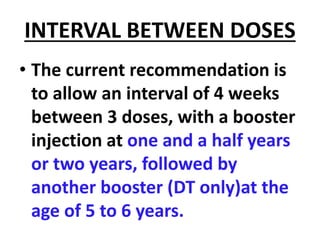
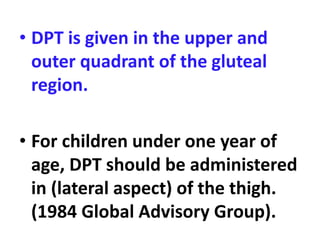
Diphtheria is caused by Corynebacterium diphtheriae which produces a toxin. It typically affects the throat and tonsils, forming a gray membrane. The toxin can also damage organs like the heart. It is spread through respiratory droplets or skin lesions. Children under 5 are most commonly affected. Control measures include early detection, isolation, treatment with antitoxin and antibiotics, and active immunization with DPT vaccine starting at 6 weeks of age with booster doses. Prompt treatment and immunization have greatly reduced the incidence of diphtheria.