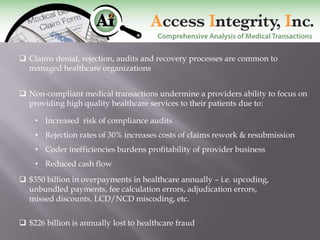
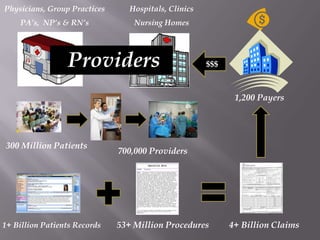
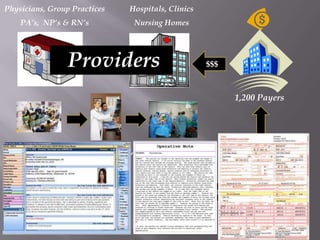
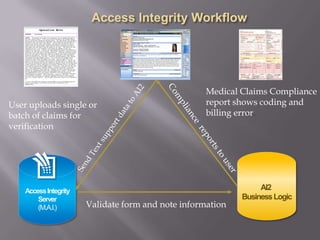
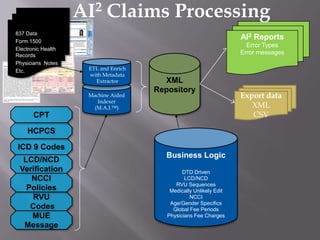
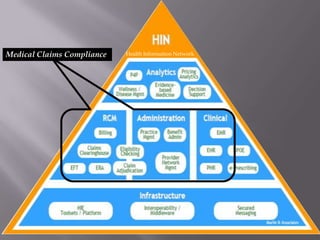
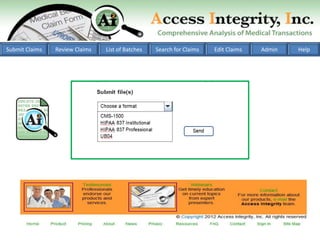
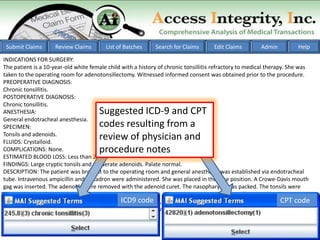
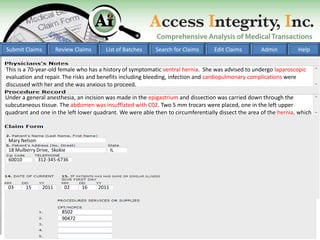
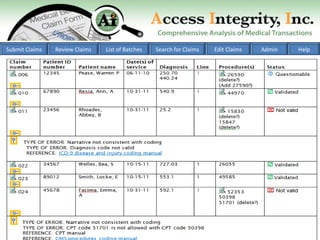
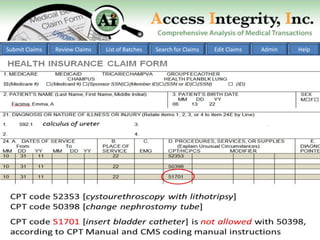
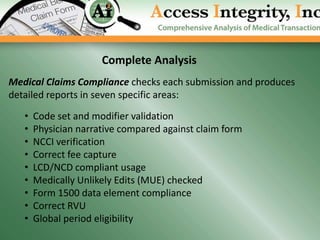
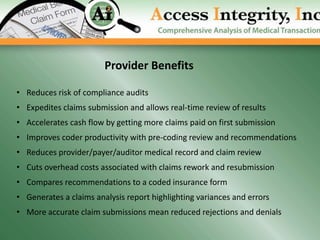
The document discusses the challenges of medical claims compliance, highlighting issues such as fraud, denial rates, and the financial impact on healthcare providers. It presents a comprehensive analysis of medical transactions that employs technology to improve compliance and efficiency in claims processing. Key product features include validation of coding, fee calculations, and compliance checks, aimed at reducing rework costs and expediting claims submissions.