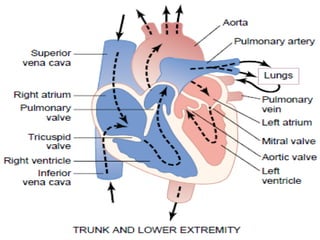
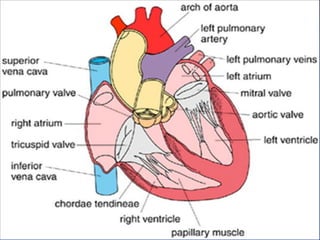
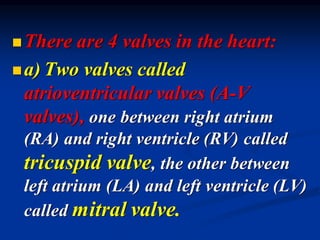
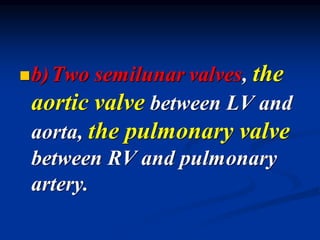
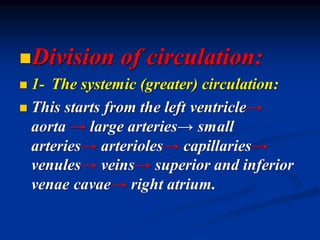
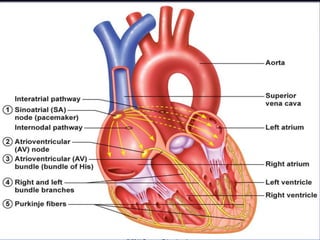
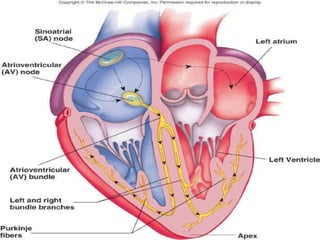
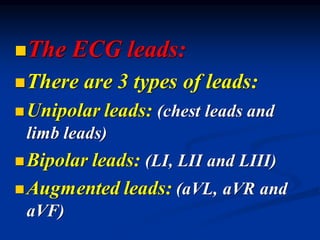
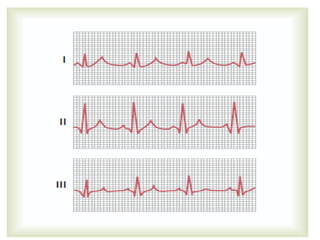
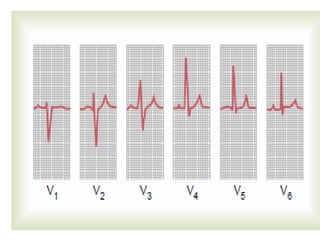
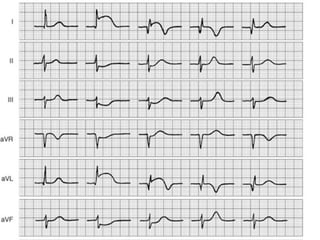
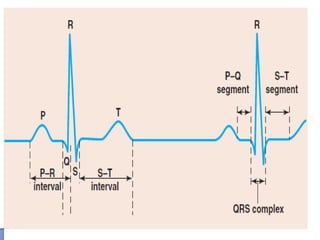
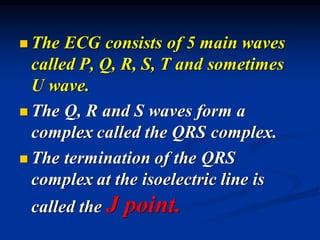
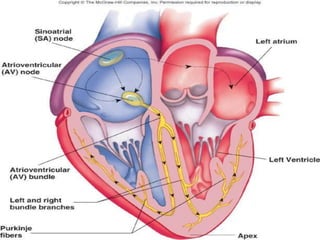
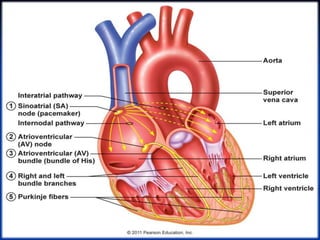
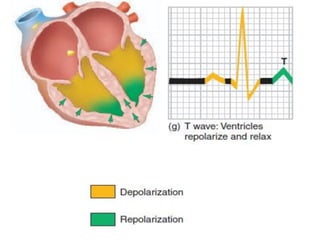
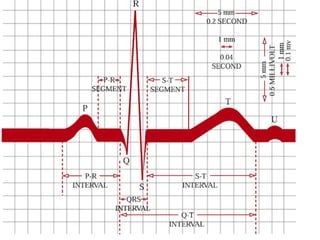
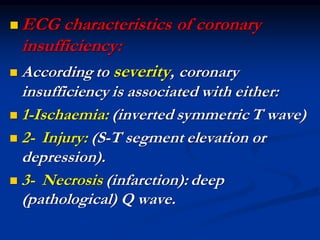
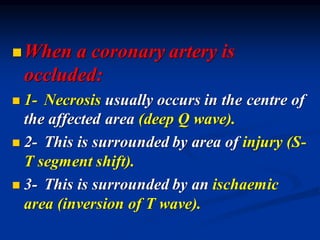
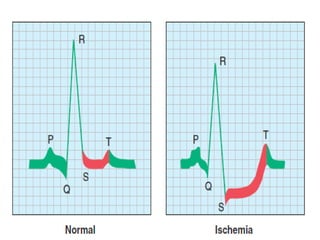
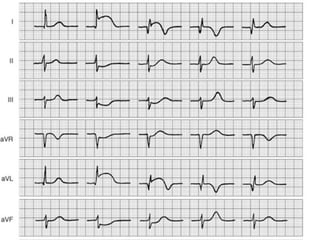
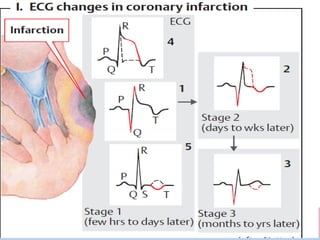
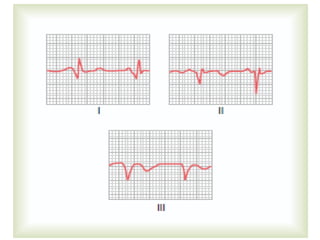
The cardiovascular system consists of the heart and blood vessels. The heart is divided into four chambers - right and left atria and ventricles. There are four valves in the heart that regulate blood flow. The circulatory system is divided into the systemic and pulmonary circulations. An electrocardiogram records and graphs the electrical activity of the heart over time and is useful for diagnosing cardiovascular conditions.