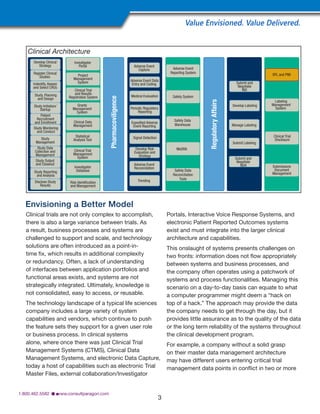
The document discusses the increasing complexity of managing clinical trials and the need for life sciences companies to improve efficiency. It notes that companies have built inefficient processes over time and acquired disparate systems through mergers and acquisitions. To meet new challenges, companies must assess their current systems and processes to identify gaps and develop a roadmap to synchronize improvements across operations and systems. Conducting a clinical architecture assessment provides a full picture of current capabilities and a path forward to optimize both systems and operations.