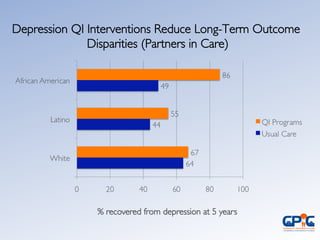
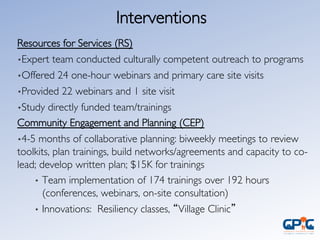
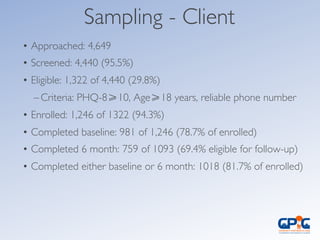
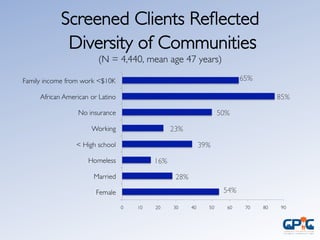
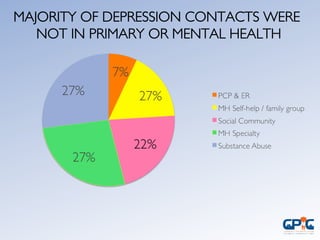
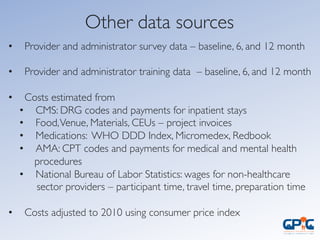
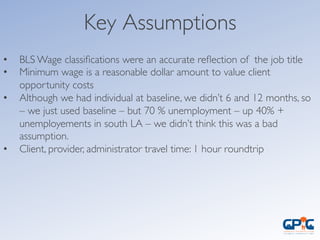
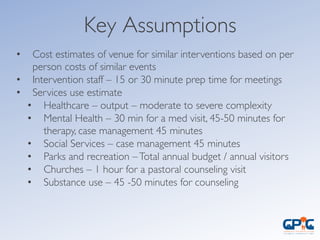
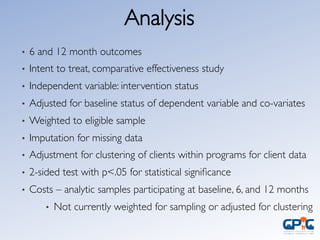
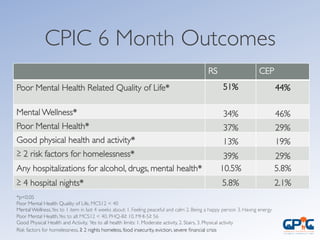
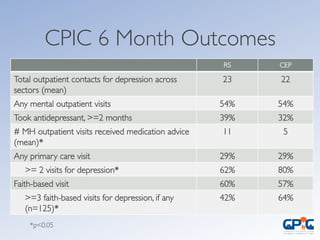
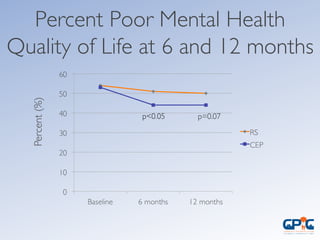
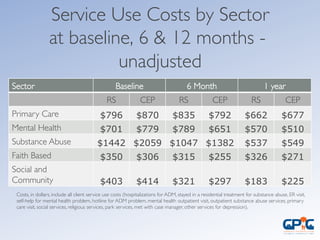
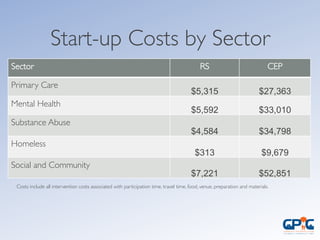
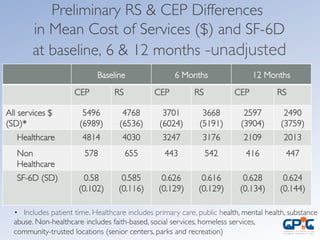
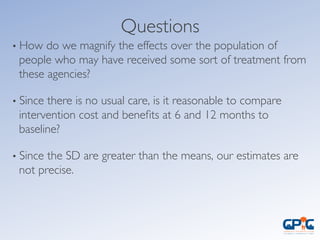
The document outlines a comparative cost analysis of depression care interventions as part of the Community Partners in Care (CPIC) initiative, highlighting the effectiveness of two implementation approaches: Resources for Services (RS) and Community Engagement and Planning (CEP). It details the outcomes related to mental health quality of life and healthcare costs over 6 and 12 months for diverse community participants while discussing the challenges faced in under-resourced areas. The analysis aims to inform better resource allocation and partnerships in addressing mental health disparities in underserved populations.