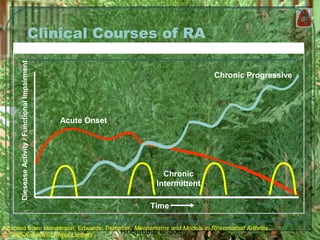
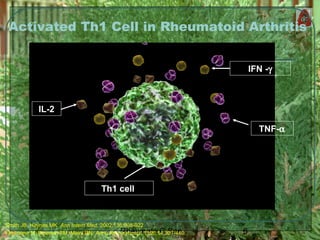
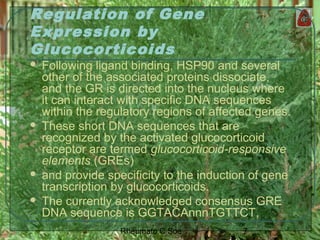
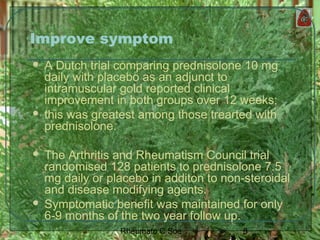
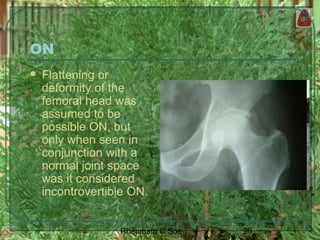
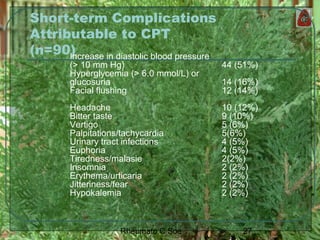
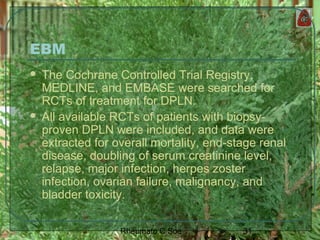
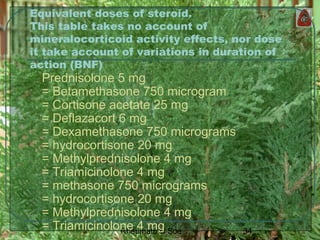
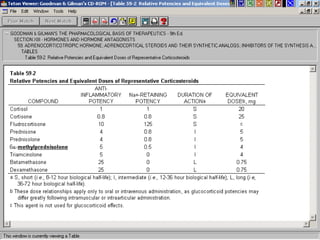
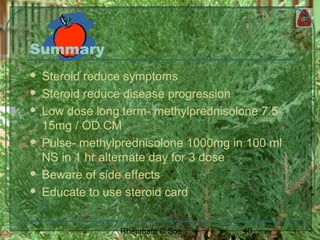
Dr. Chit Soe's document discusses the long-term use of steroids in rheumatology. It provides an overview of how steroids were initially seen as a promising treatment for rheumatoid arthritis but were later found to have serious adverse effects with high doses. The document examines the controversy around low-dose steroid use and different regimens for corticosteroid pulse therapy. It also reviews potential benefits of steroids in improving symptoms and retarding erosion, as well as common short-term and long-term side effects associated with steroid treatment.