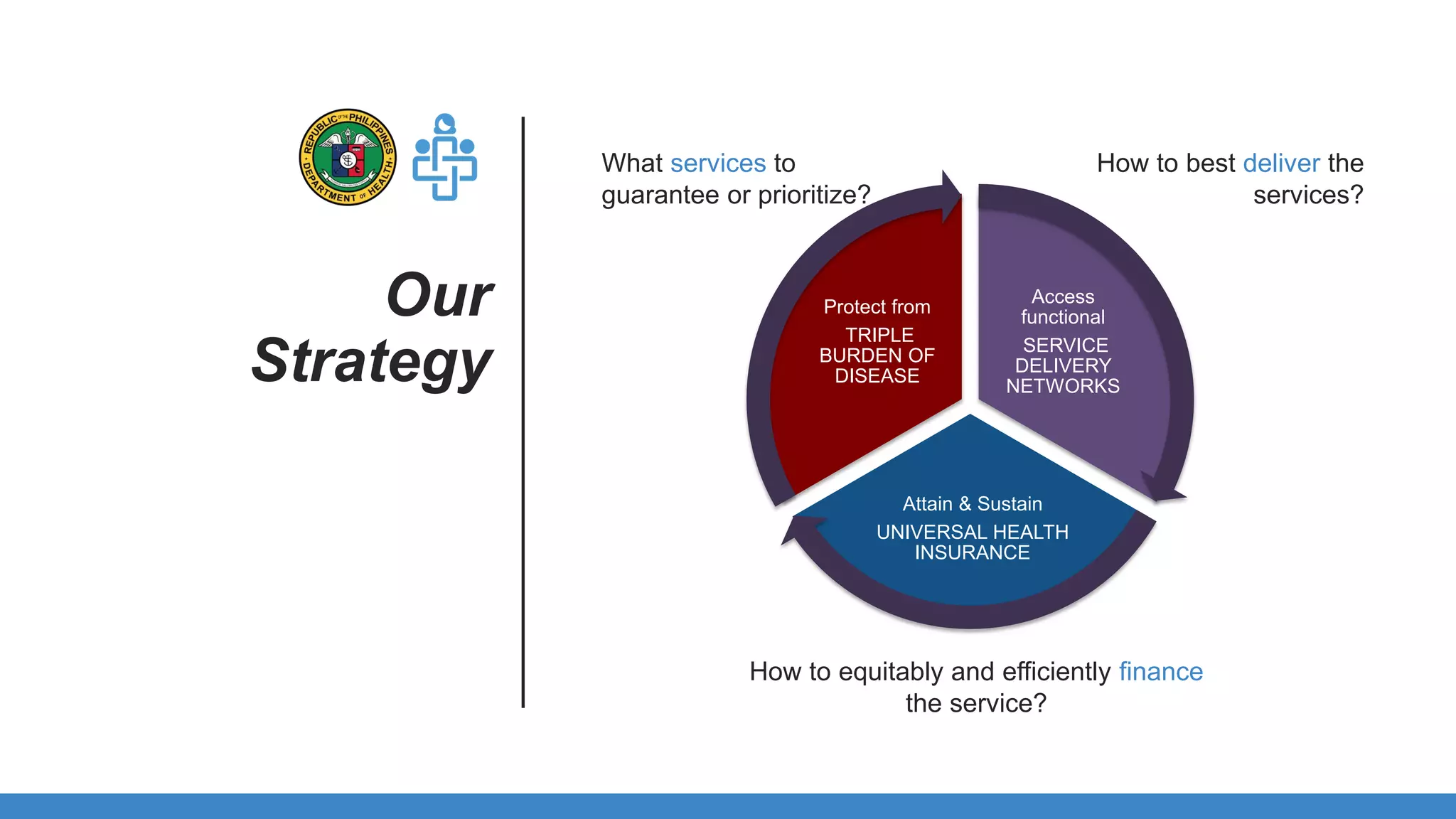
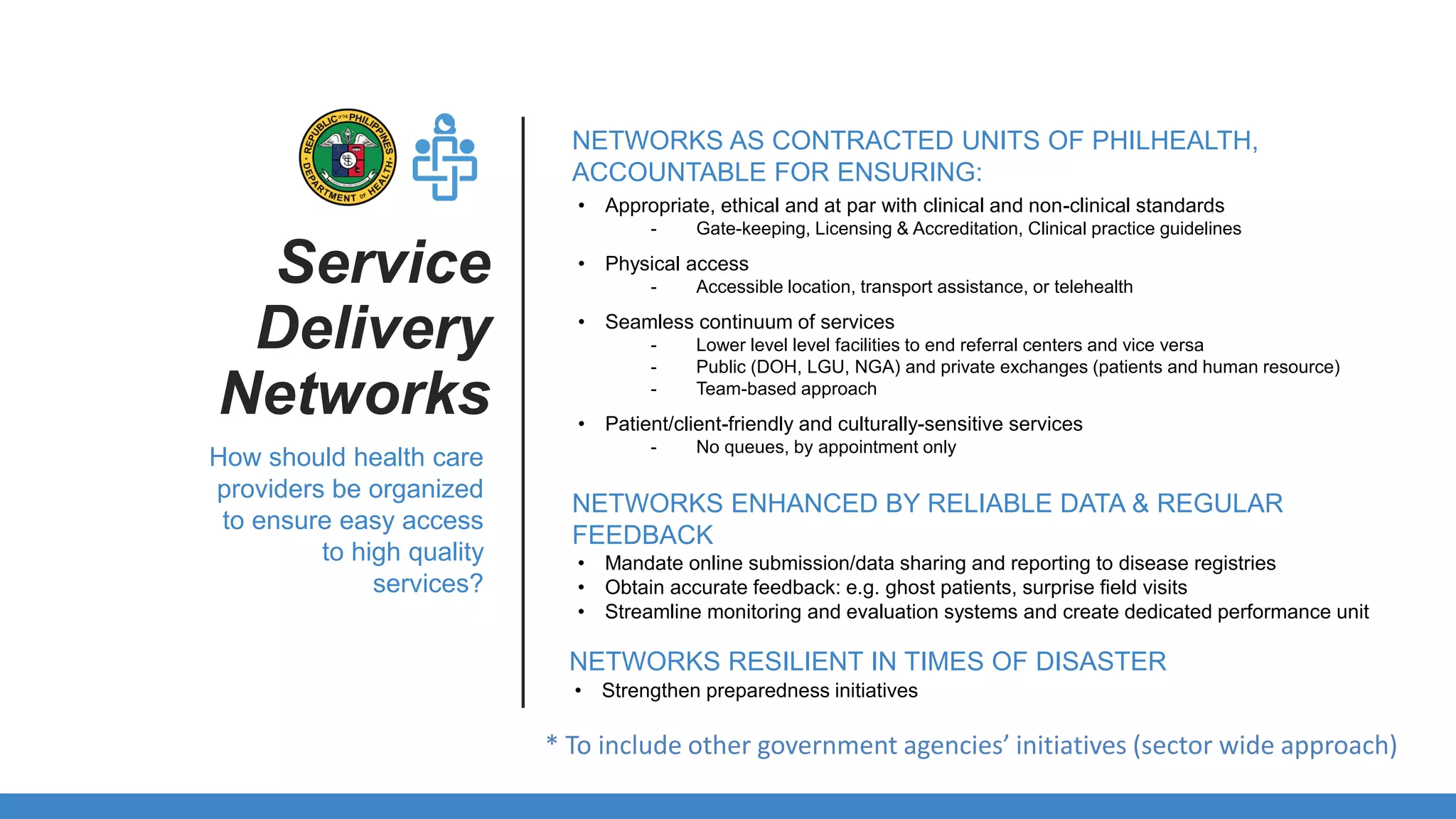
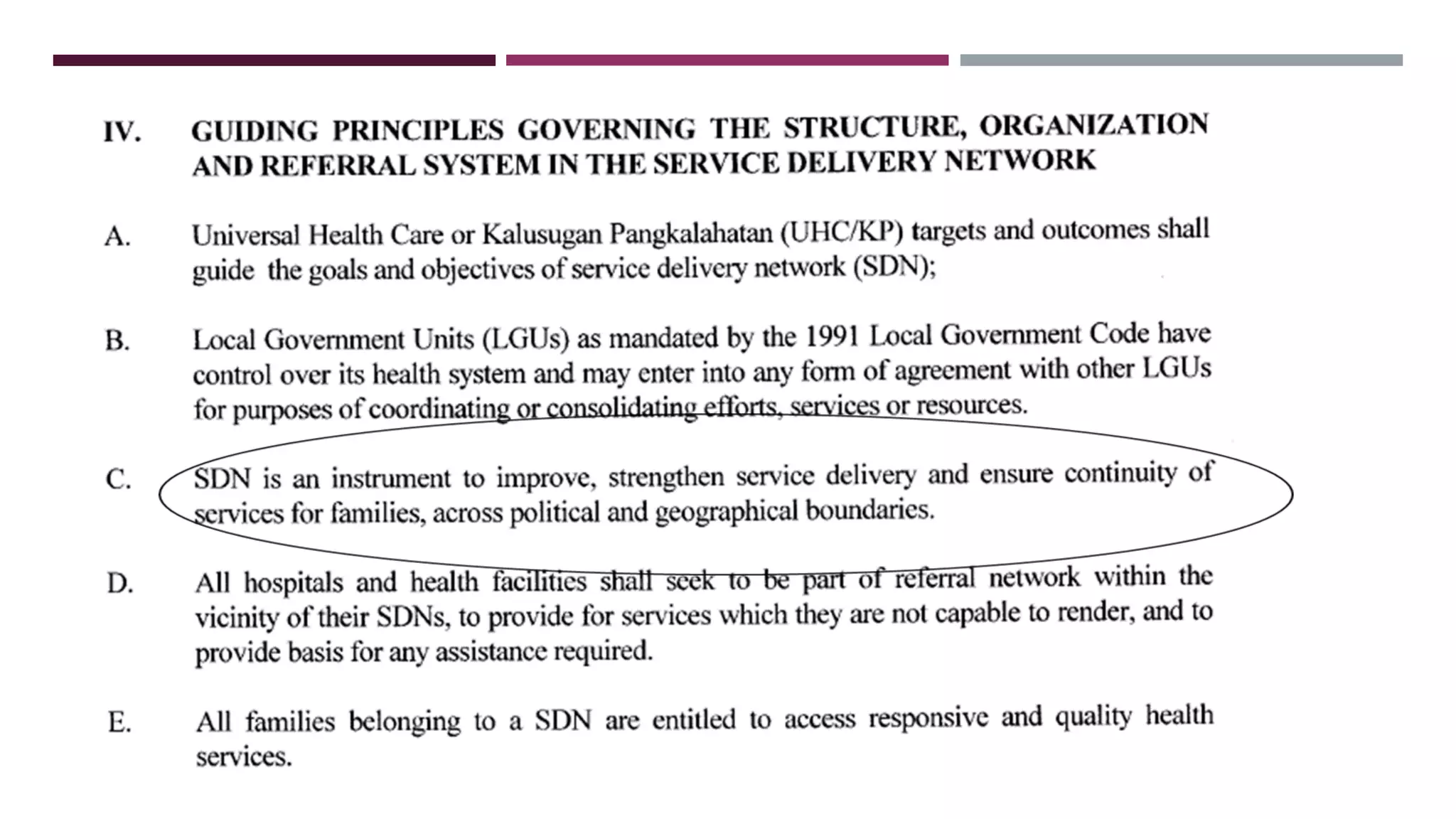
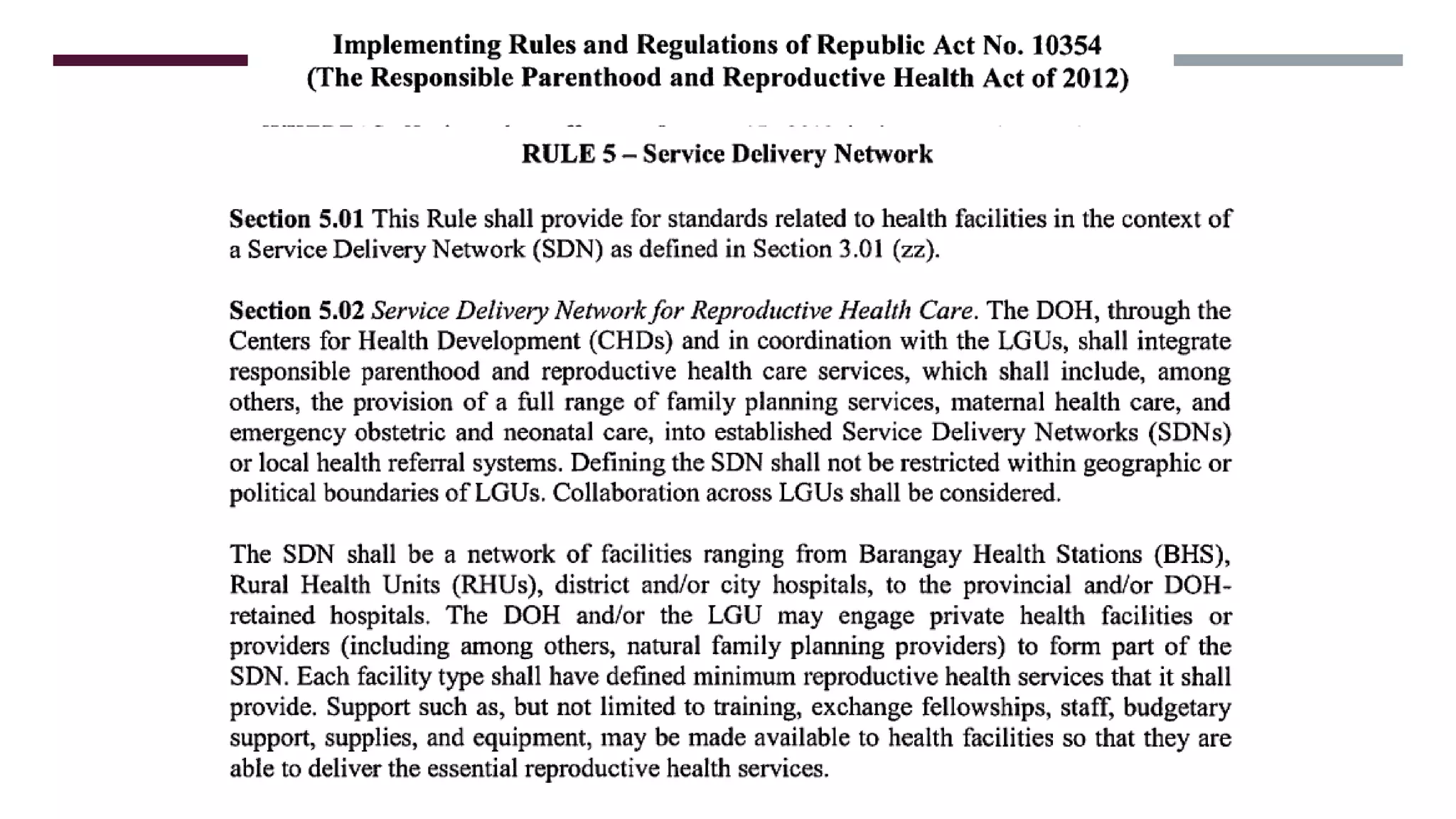
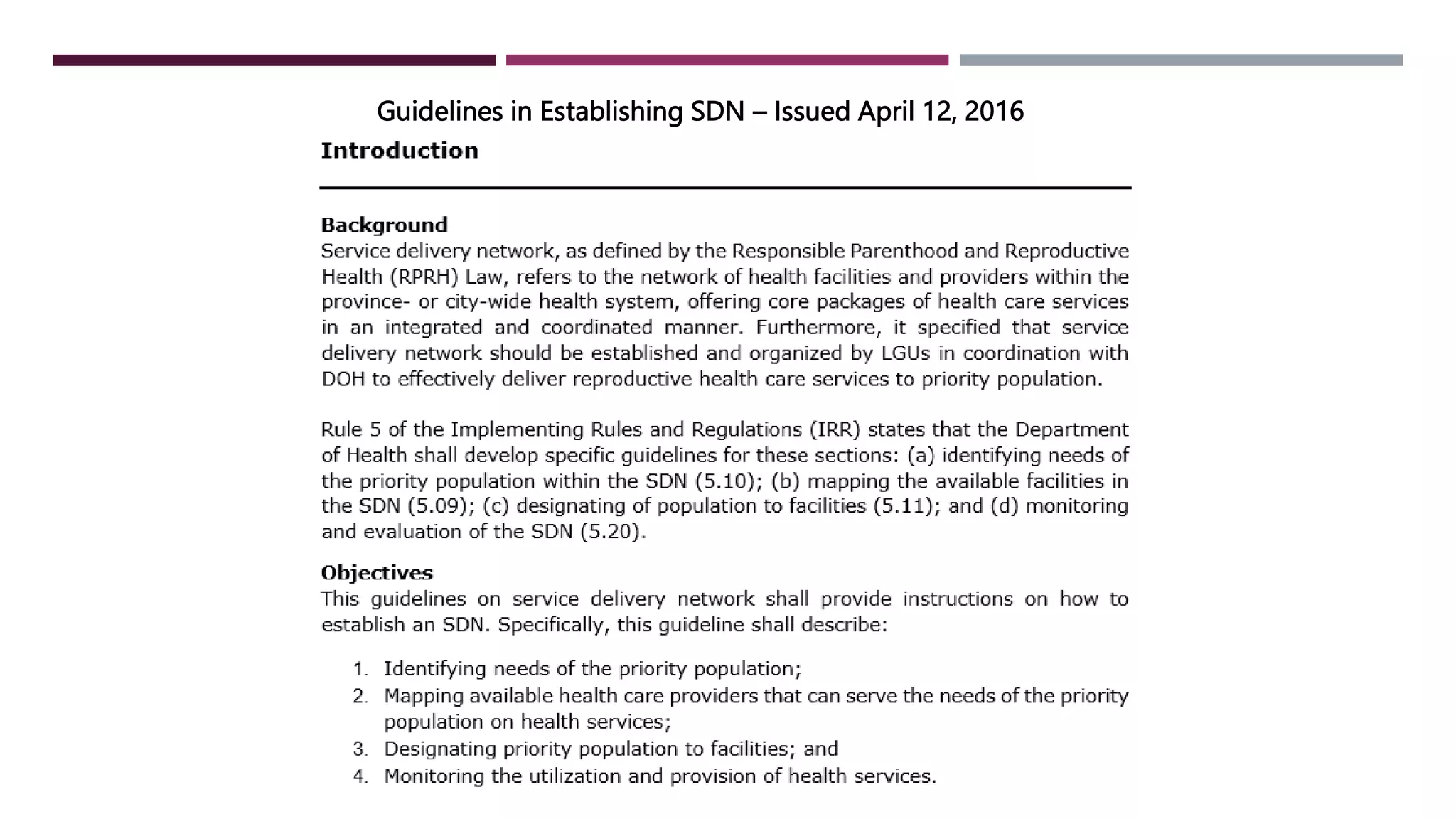
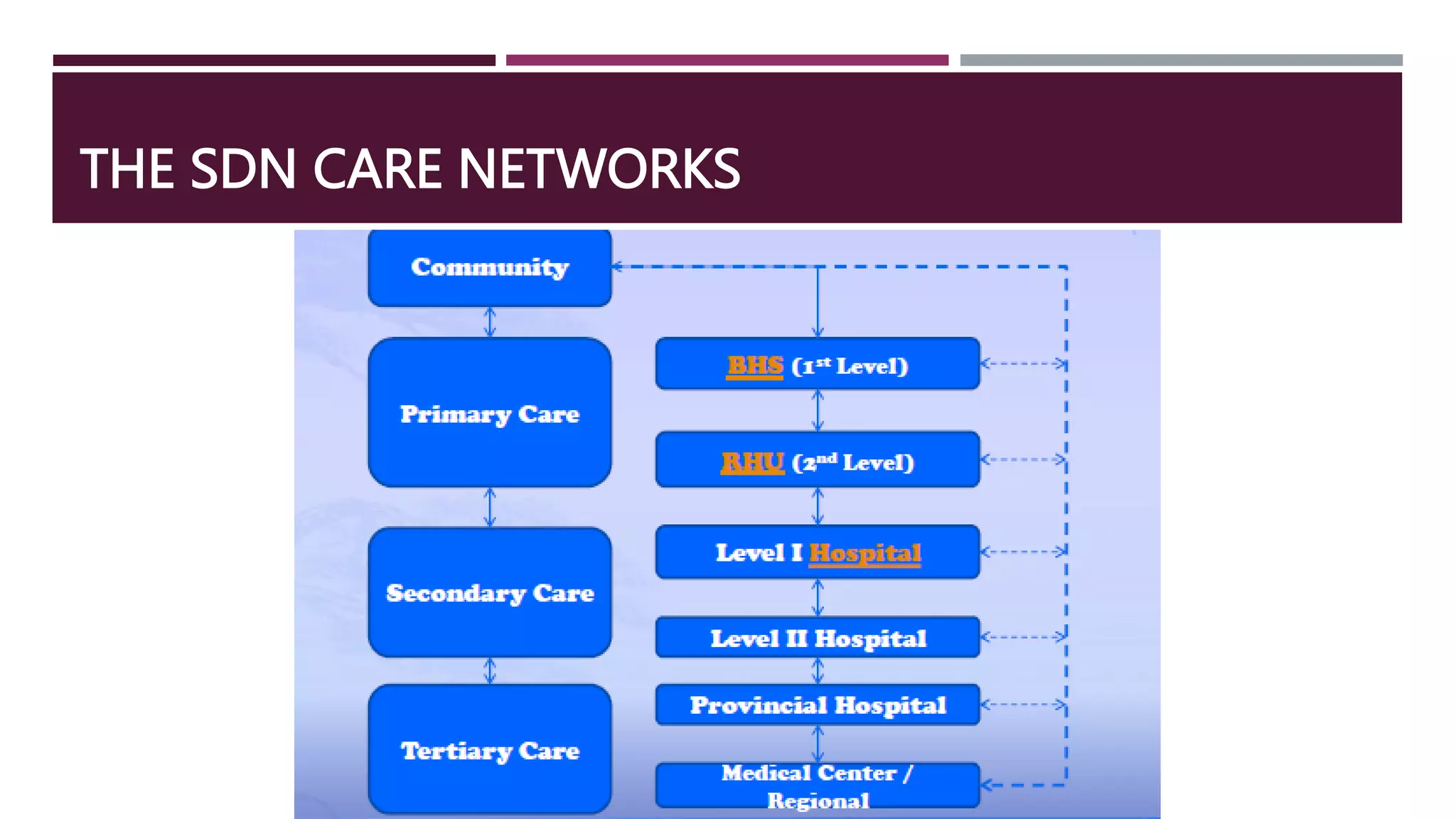
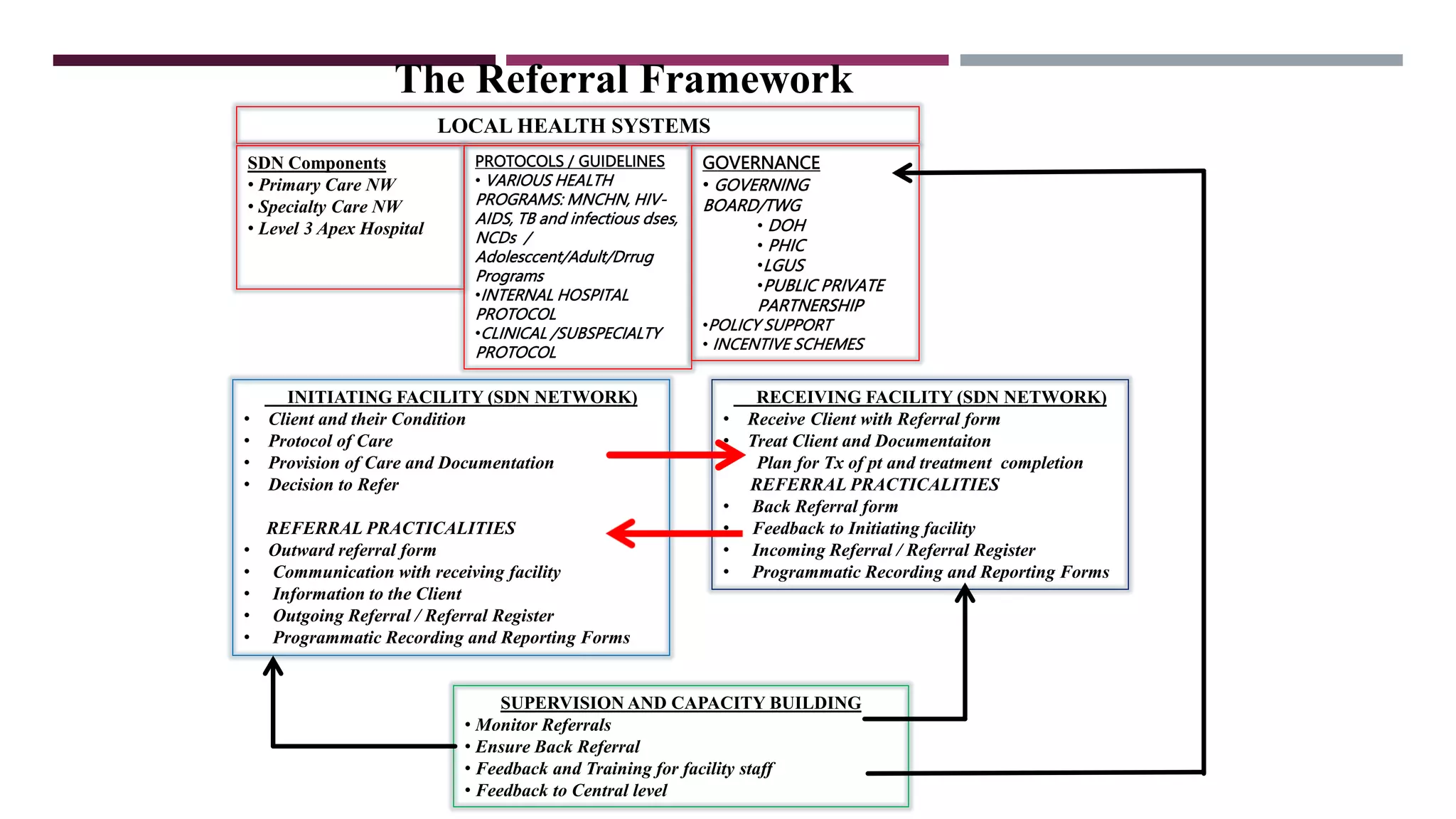
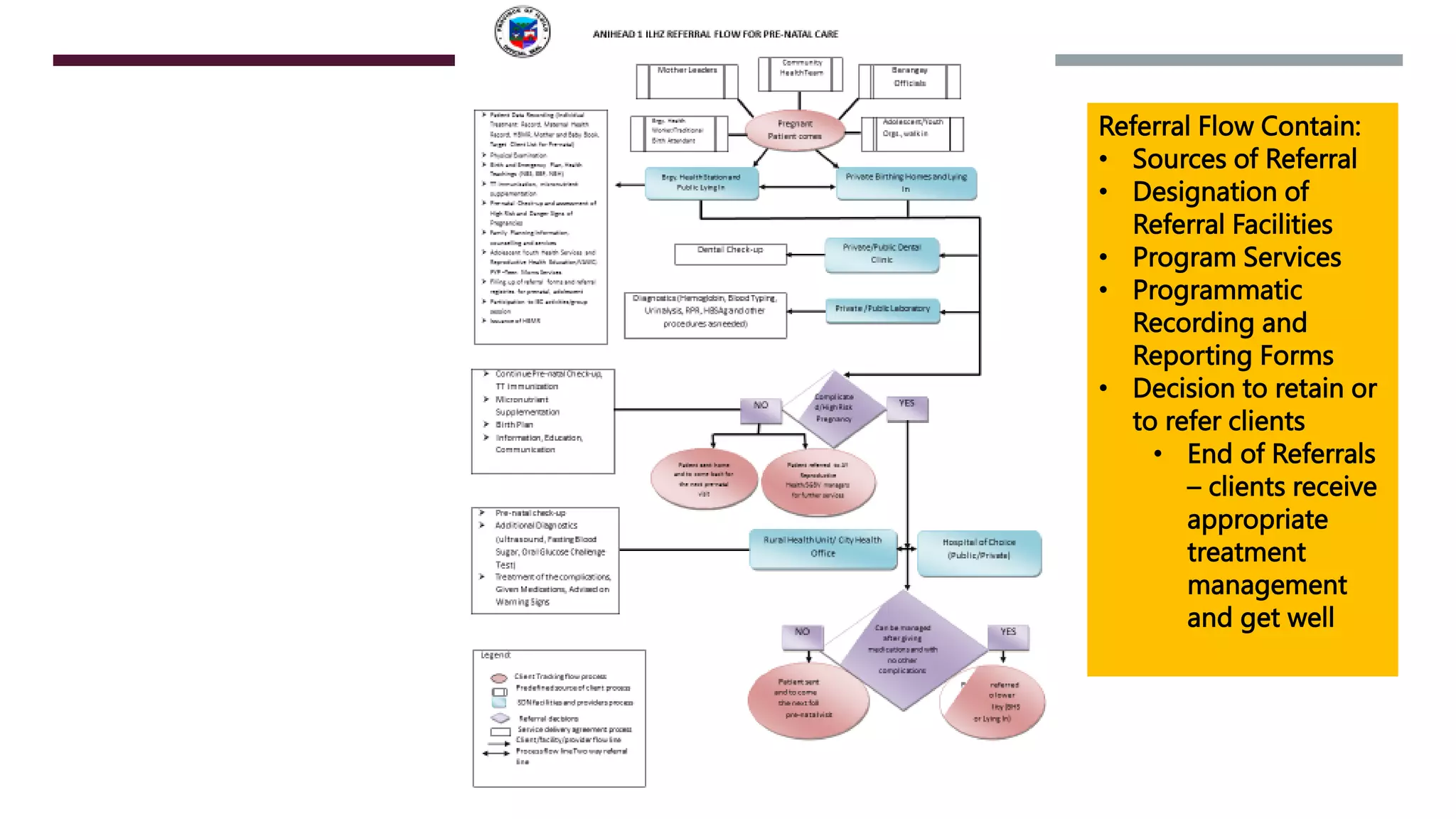
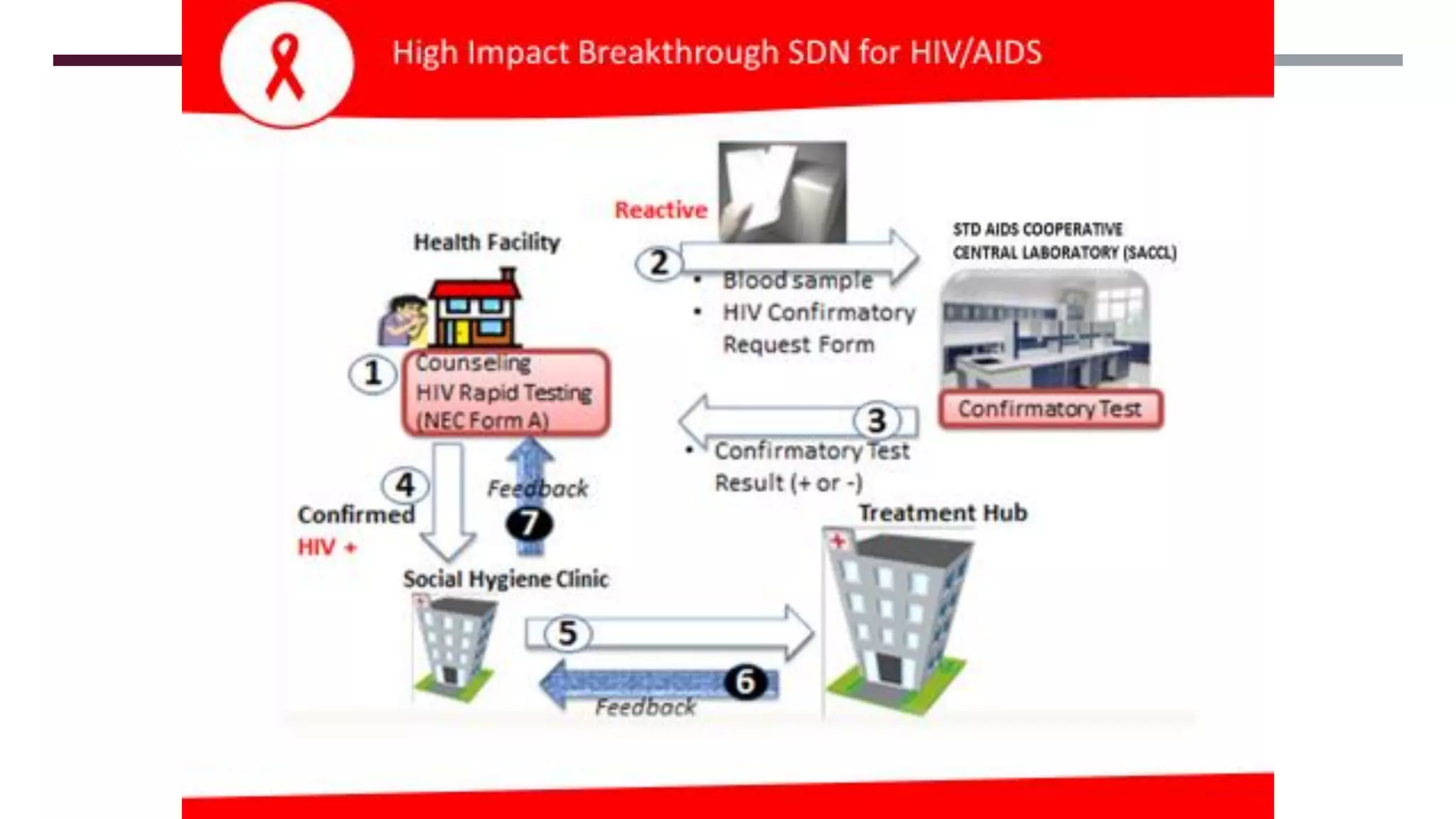
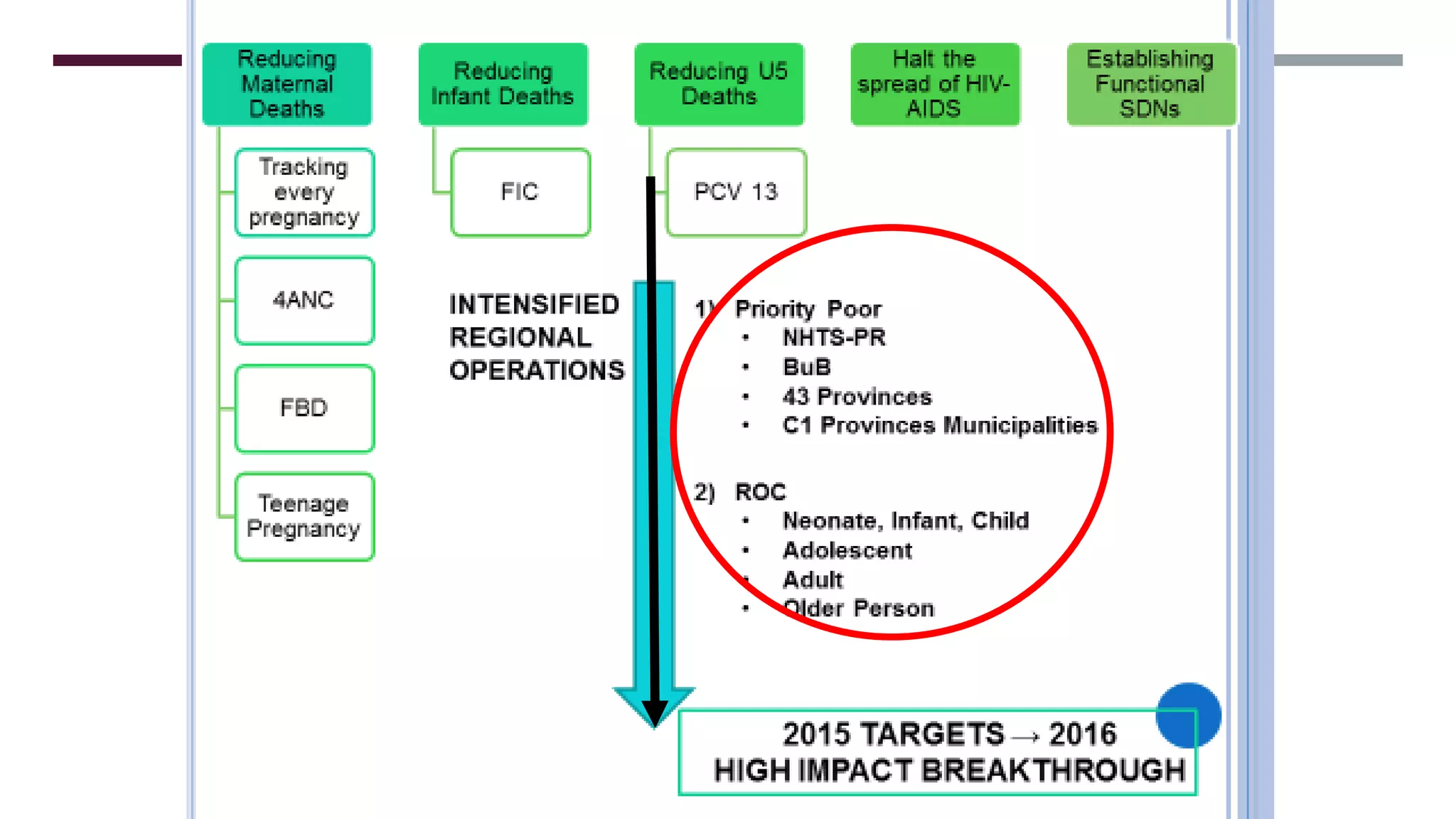
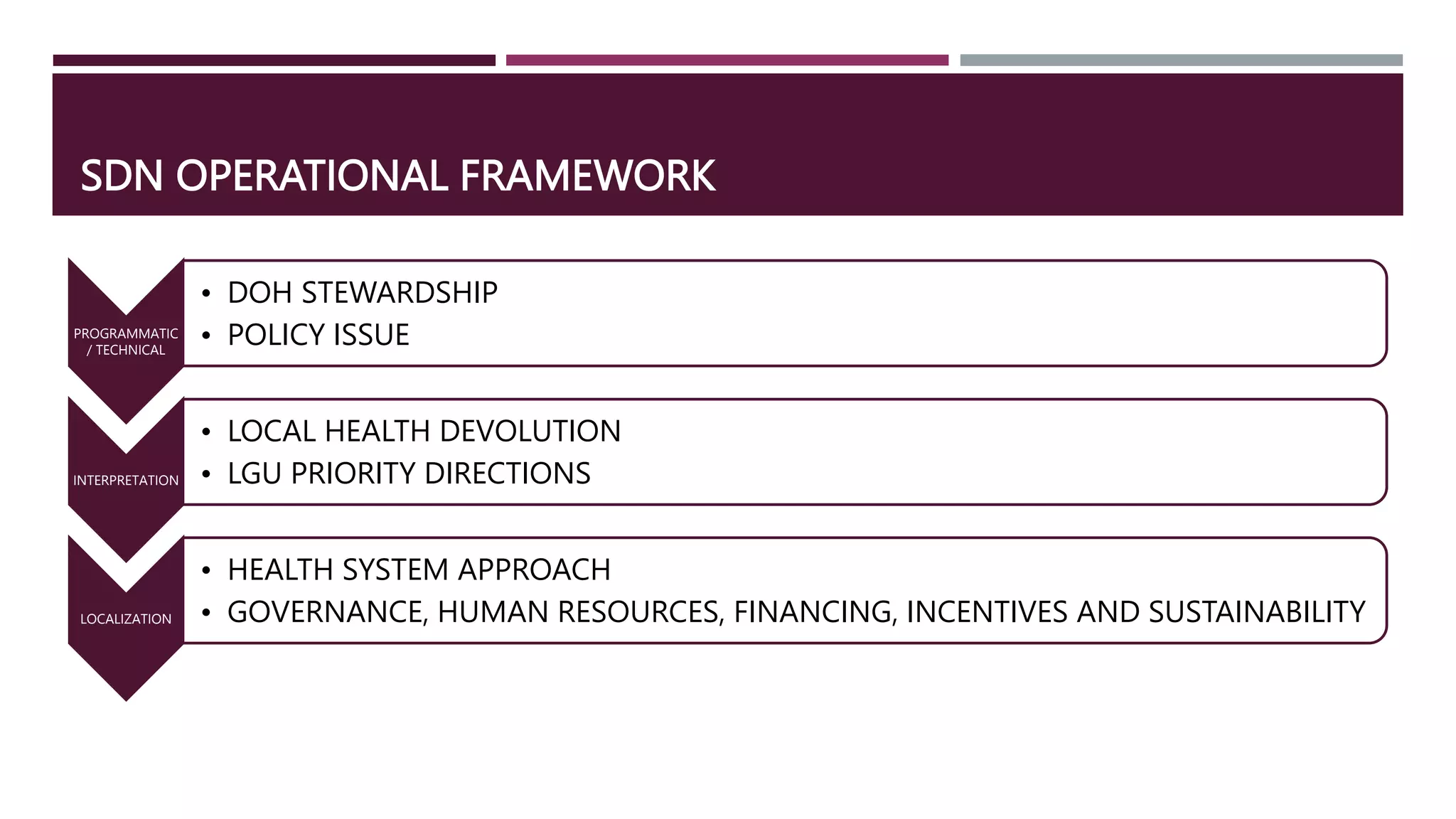
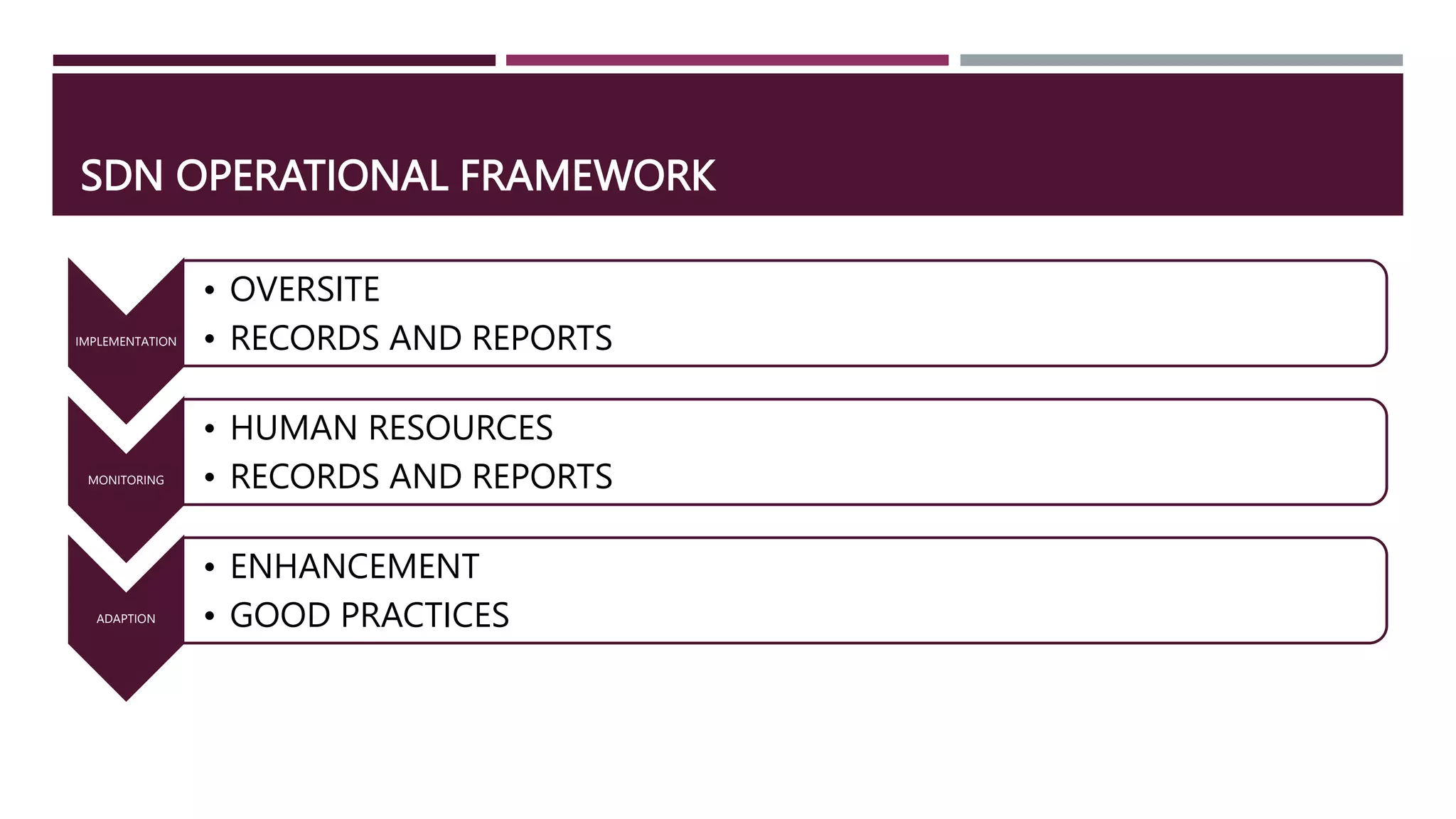
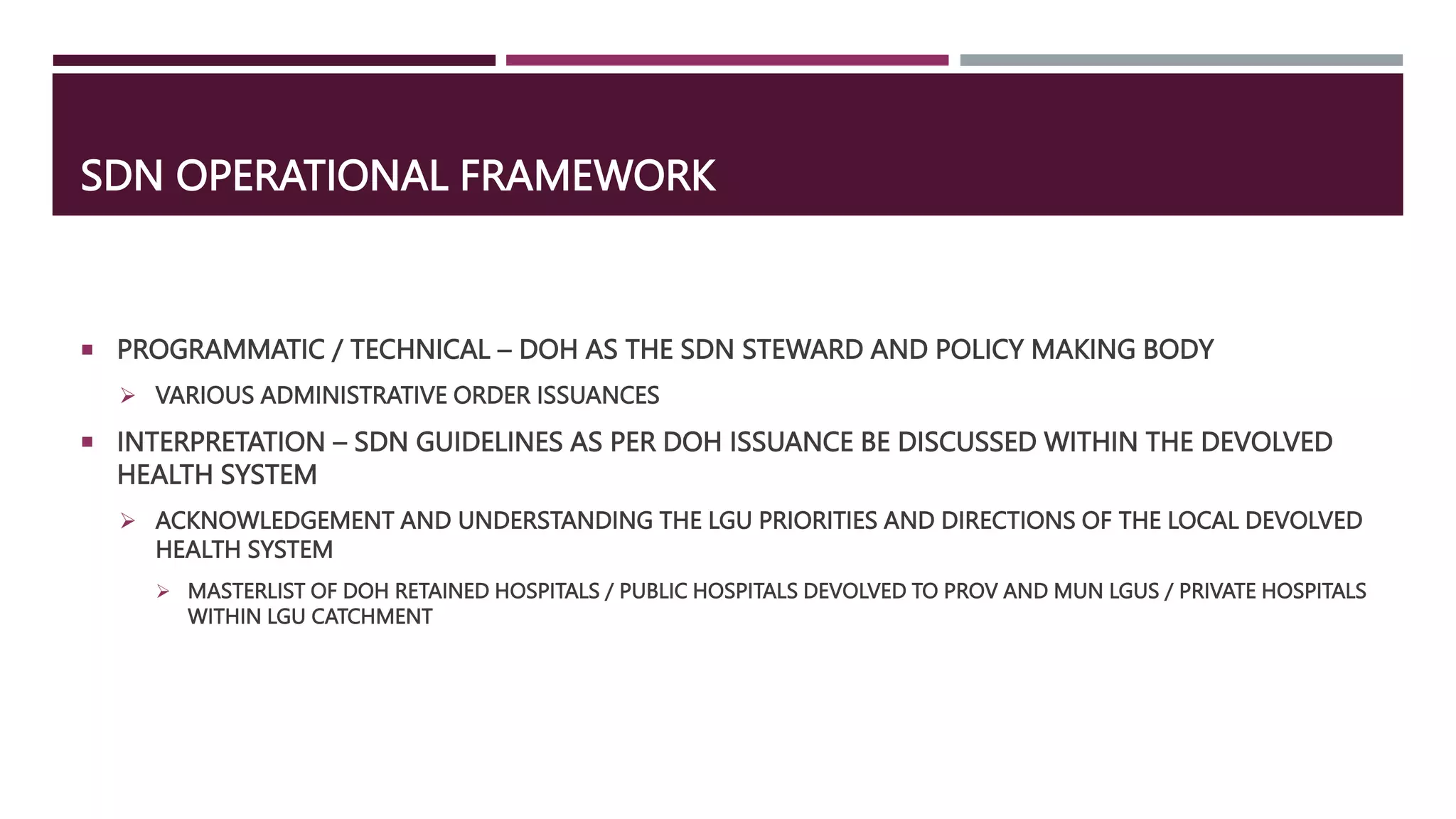
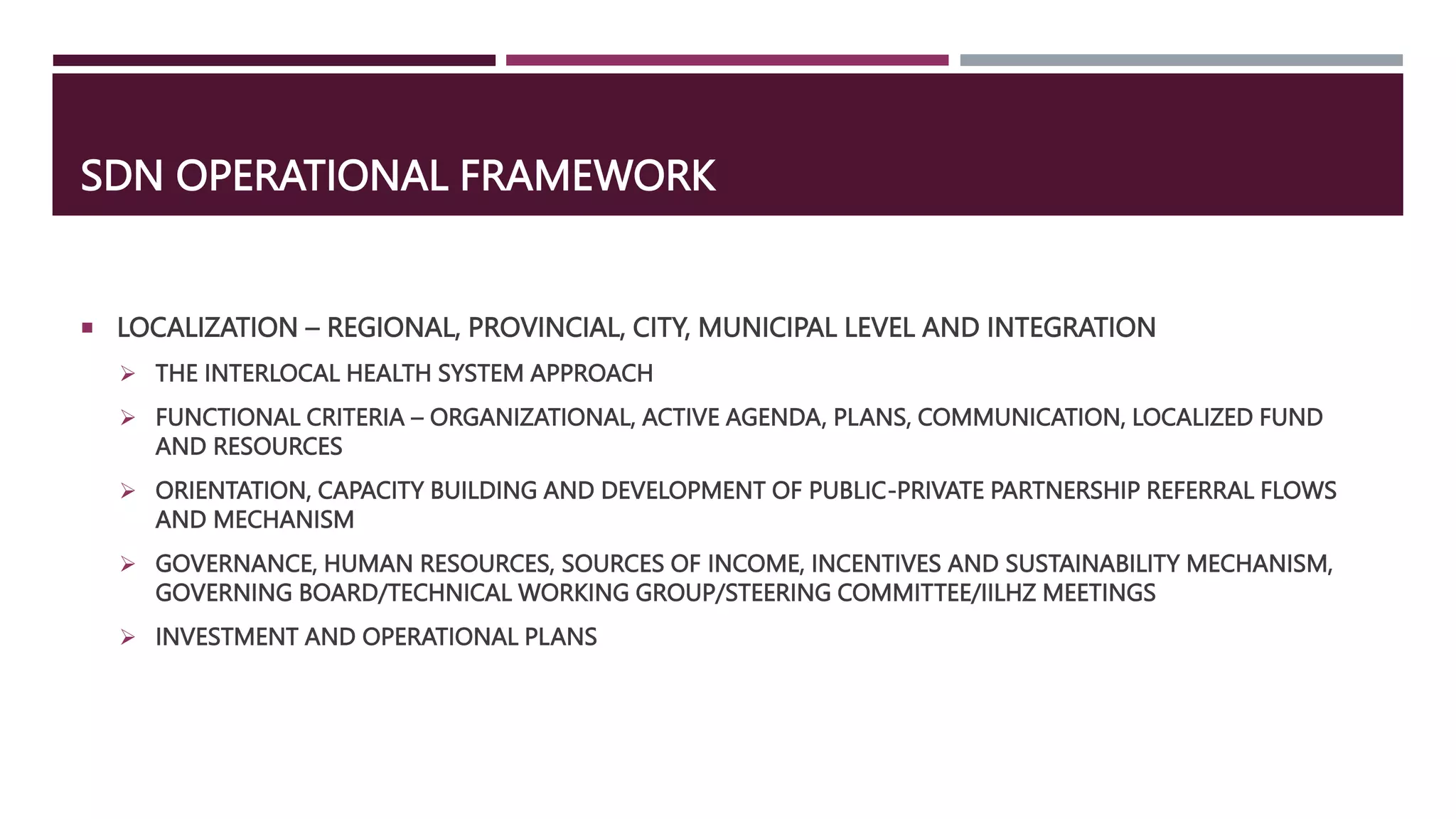
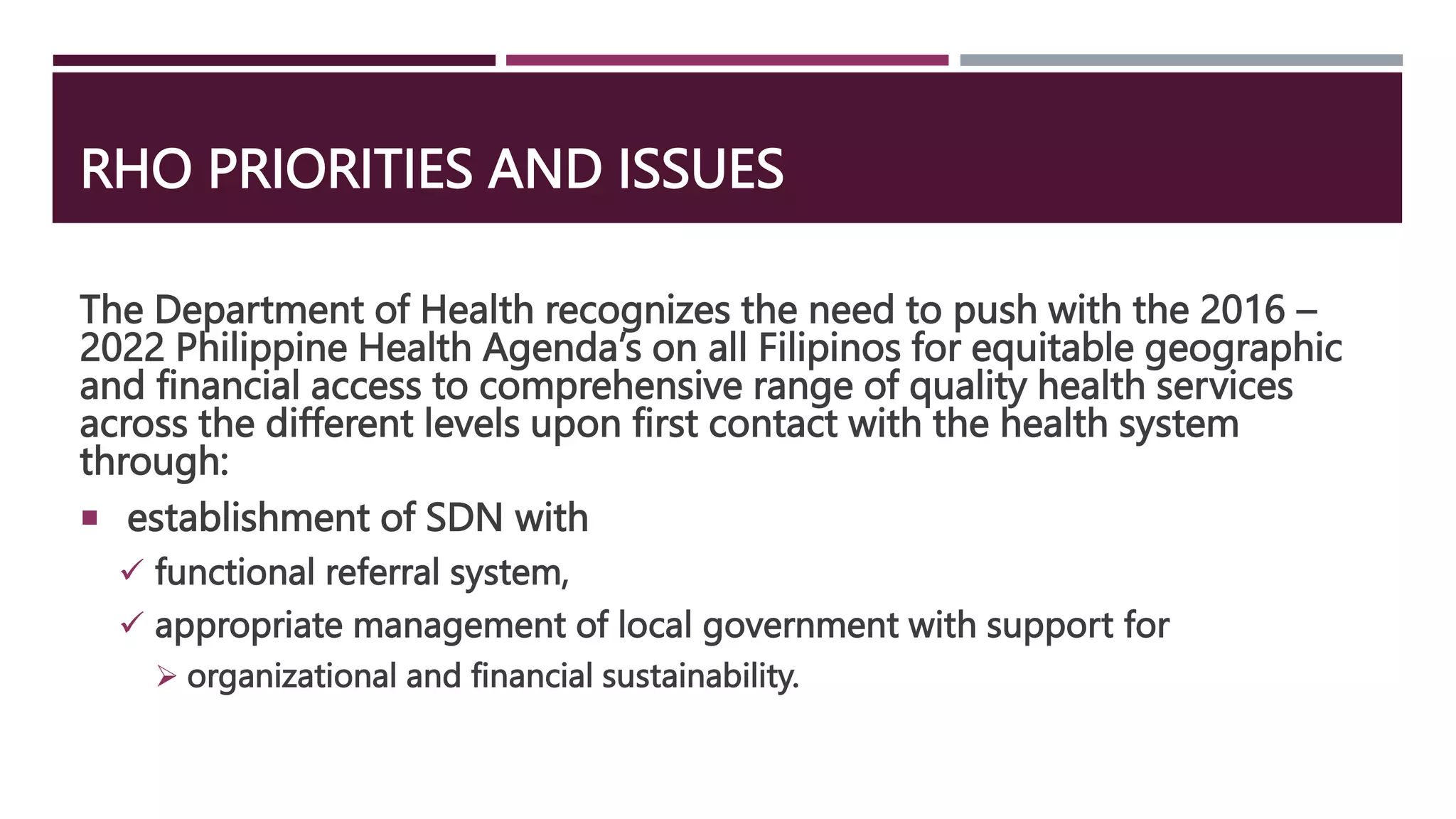
This document discusses service delivery networks (SDNs) in the context of the Philippine health system. It provides background on SDNs and their goals of improving equitable access to health services through efficient provision and continuity of care. Key points include:
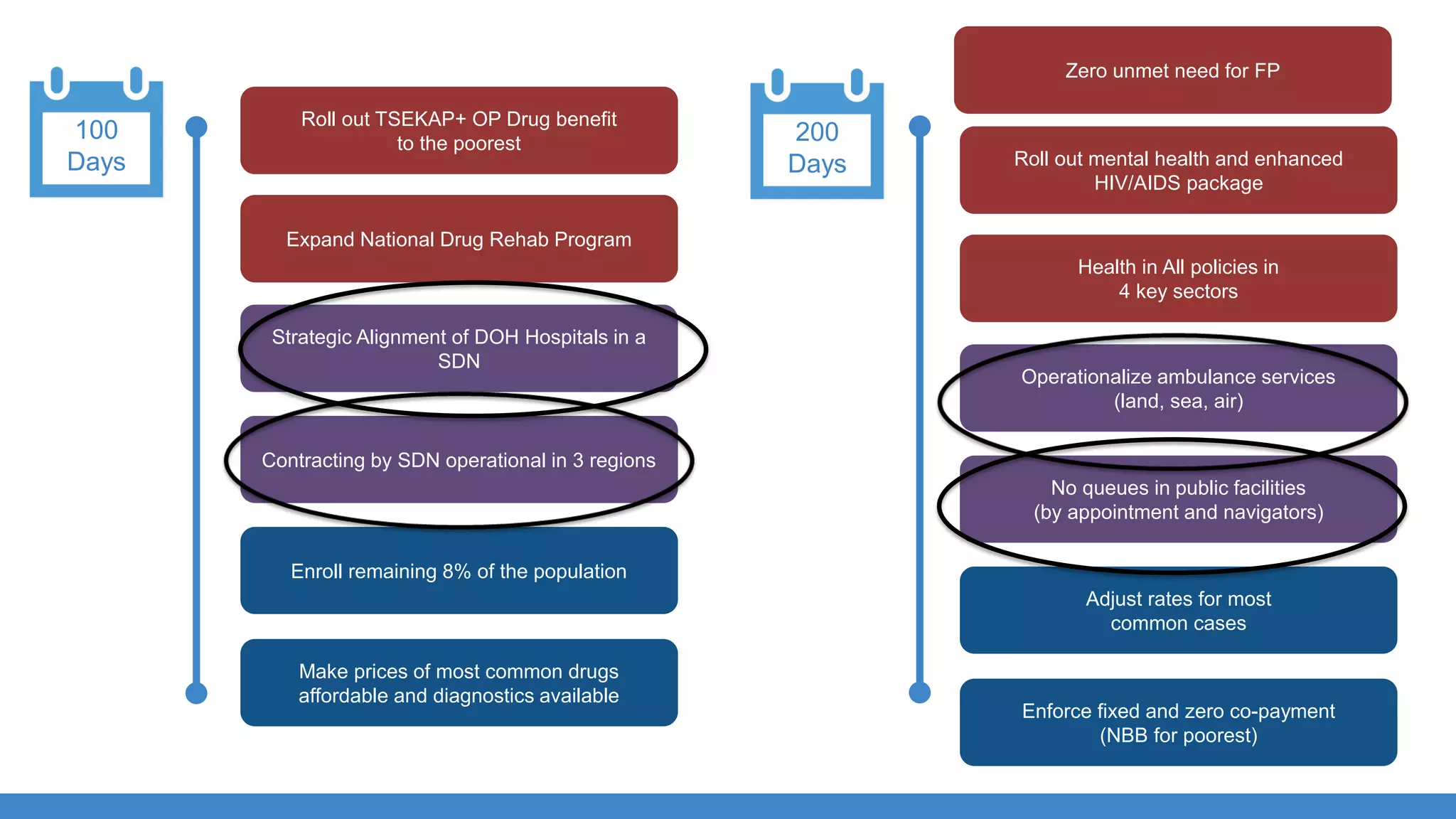
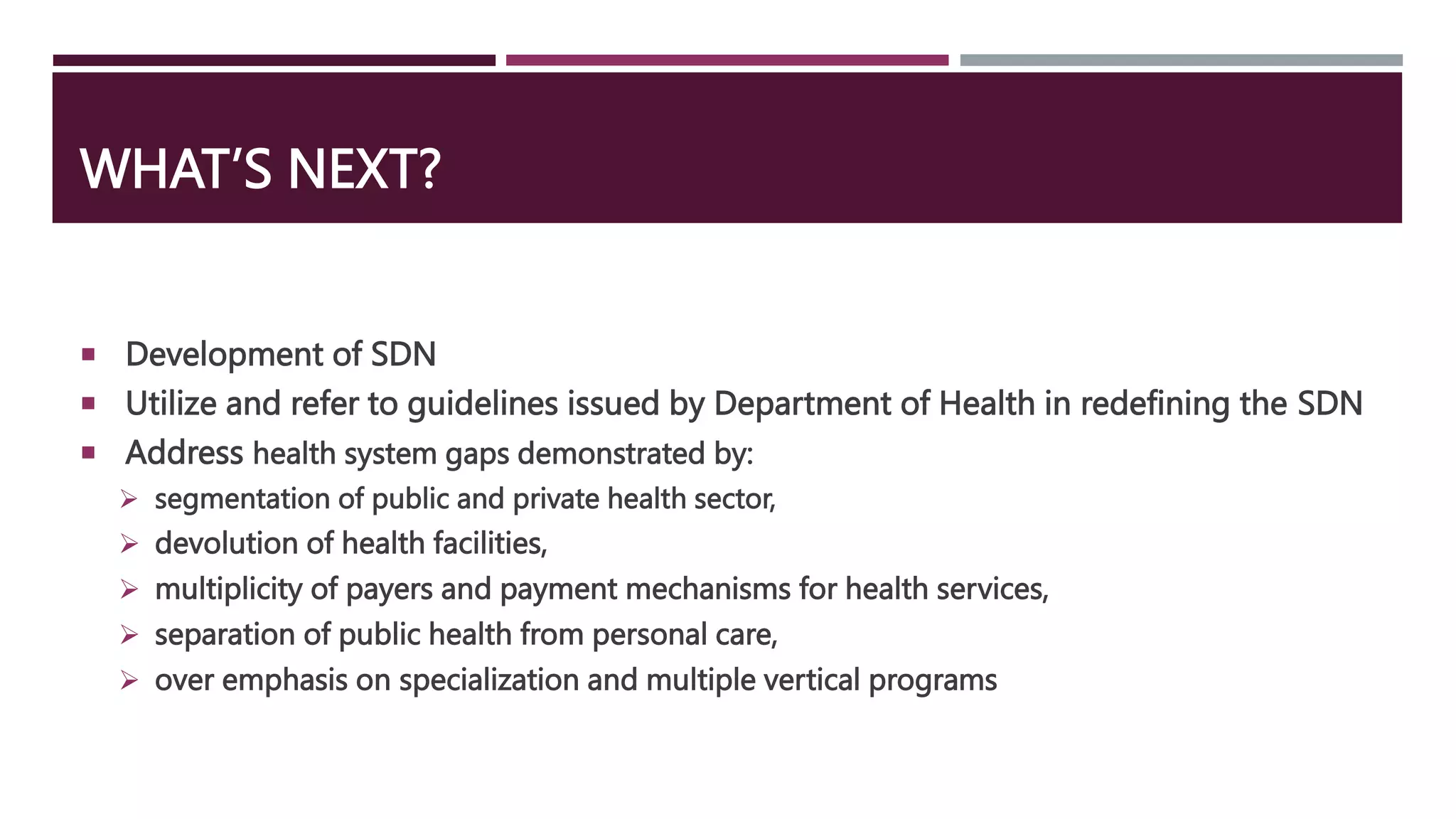
- SDNs were redefined in 2016 to better achieve universal health care goals. This involved expanding the roles of DOH, PhilHealth, LGUs and other agencies.
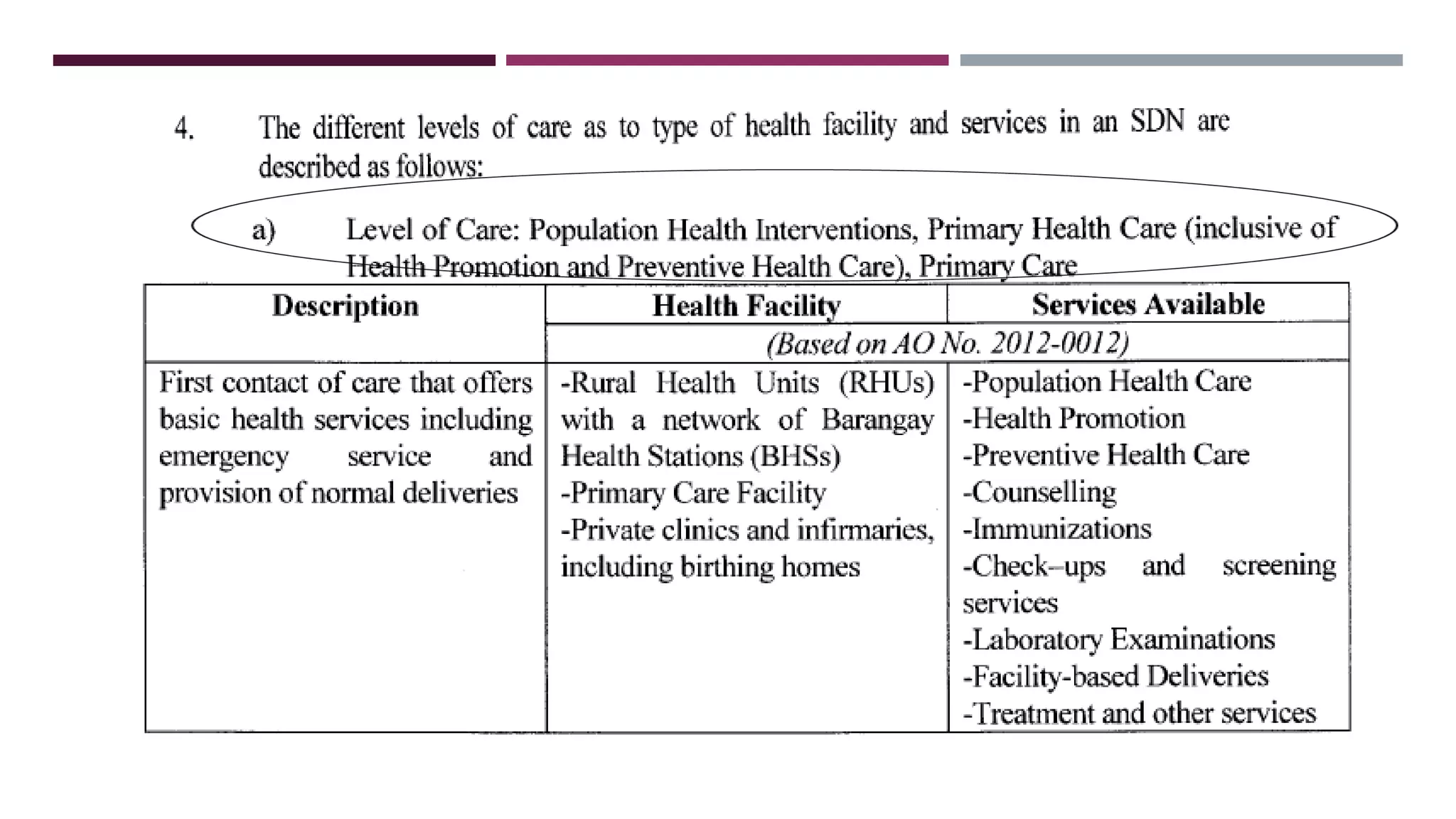
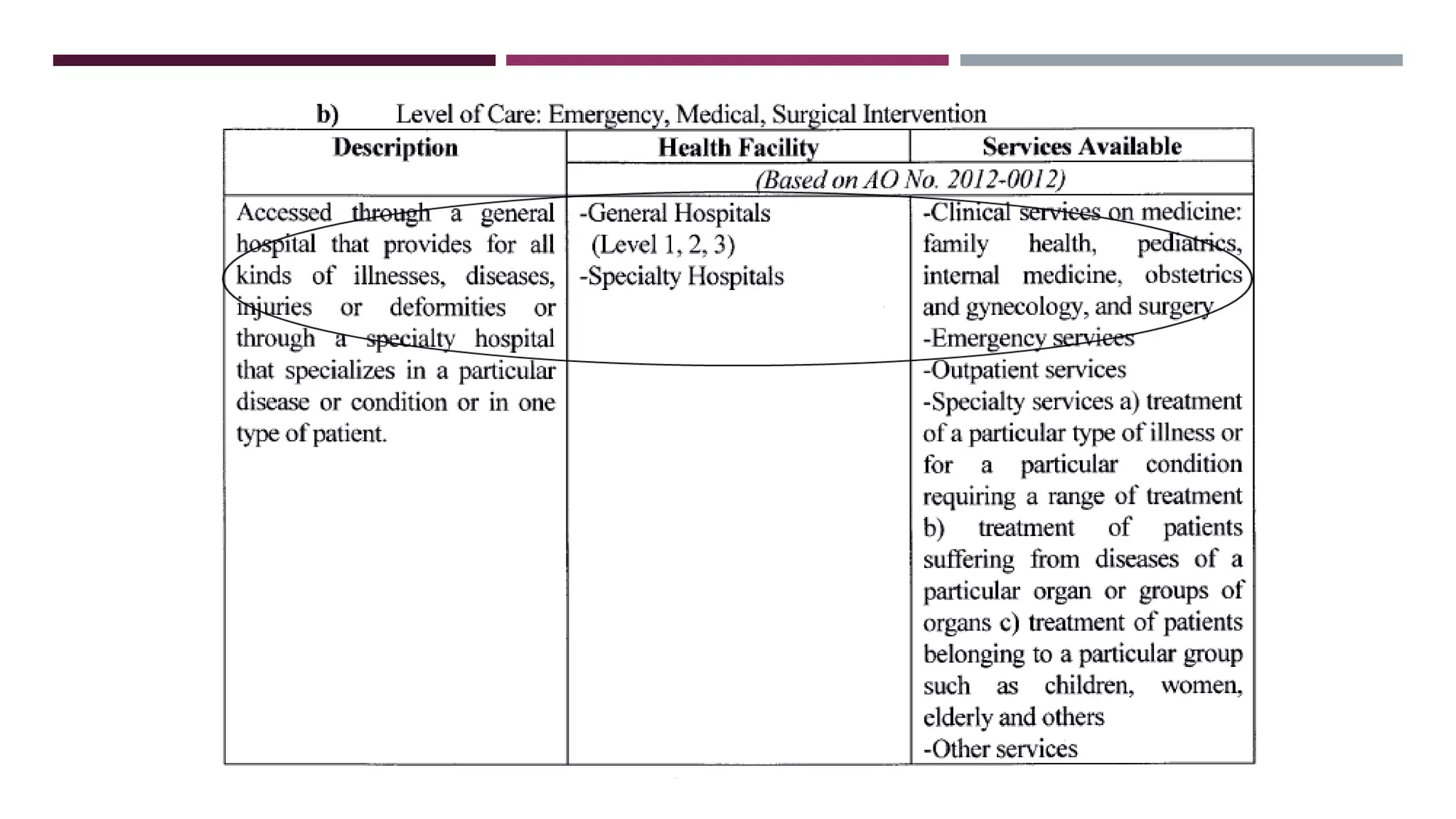
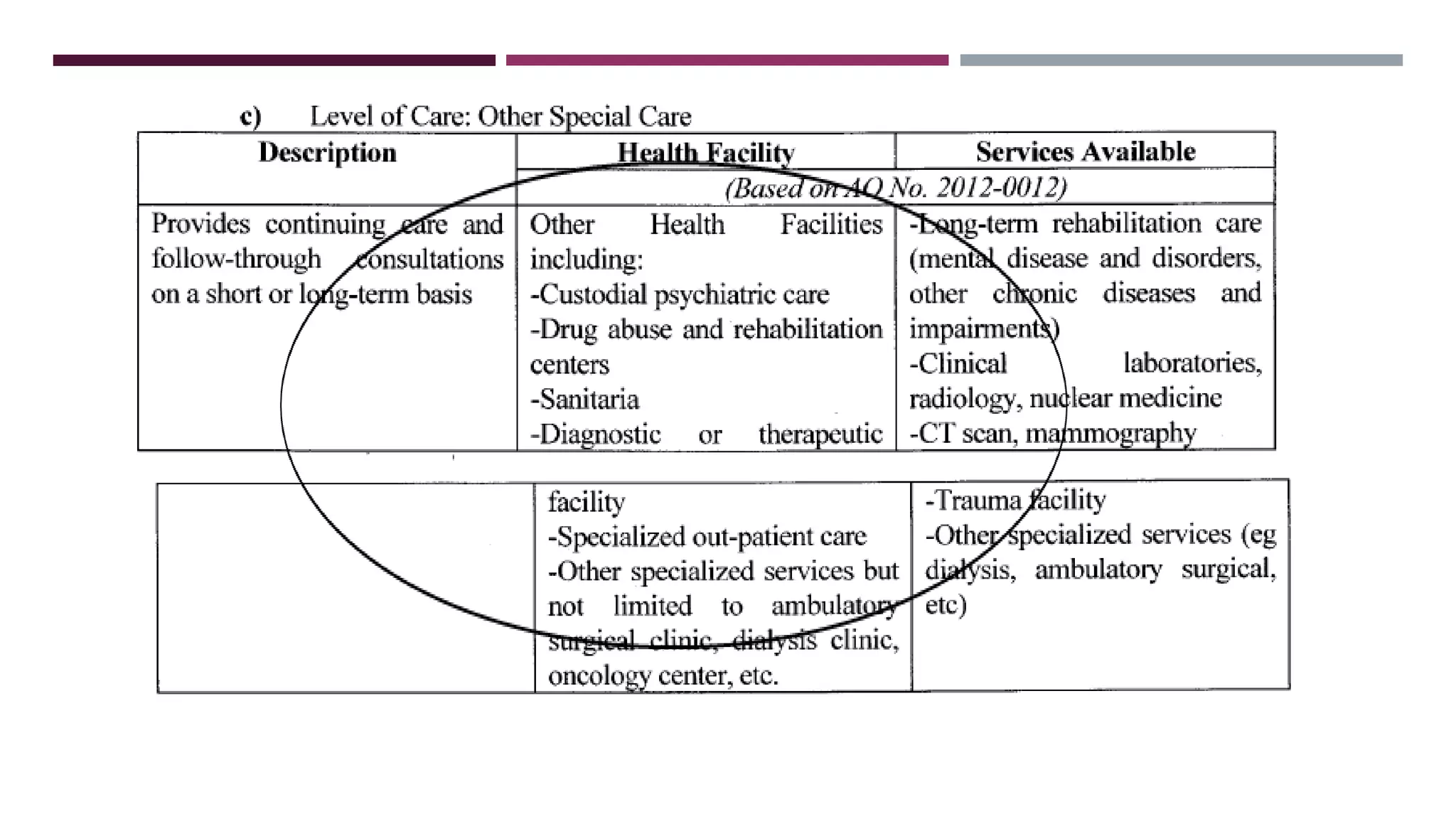
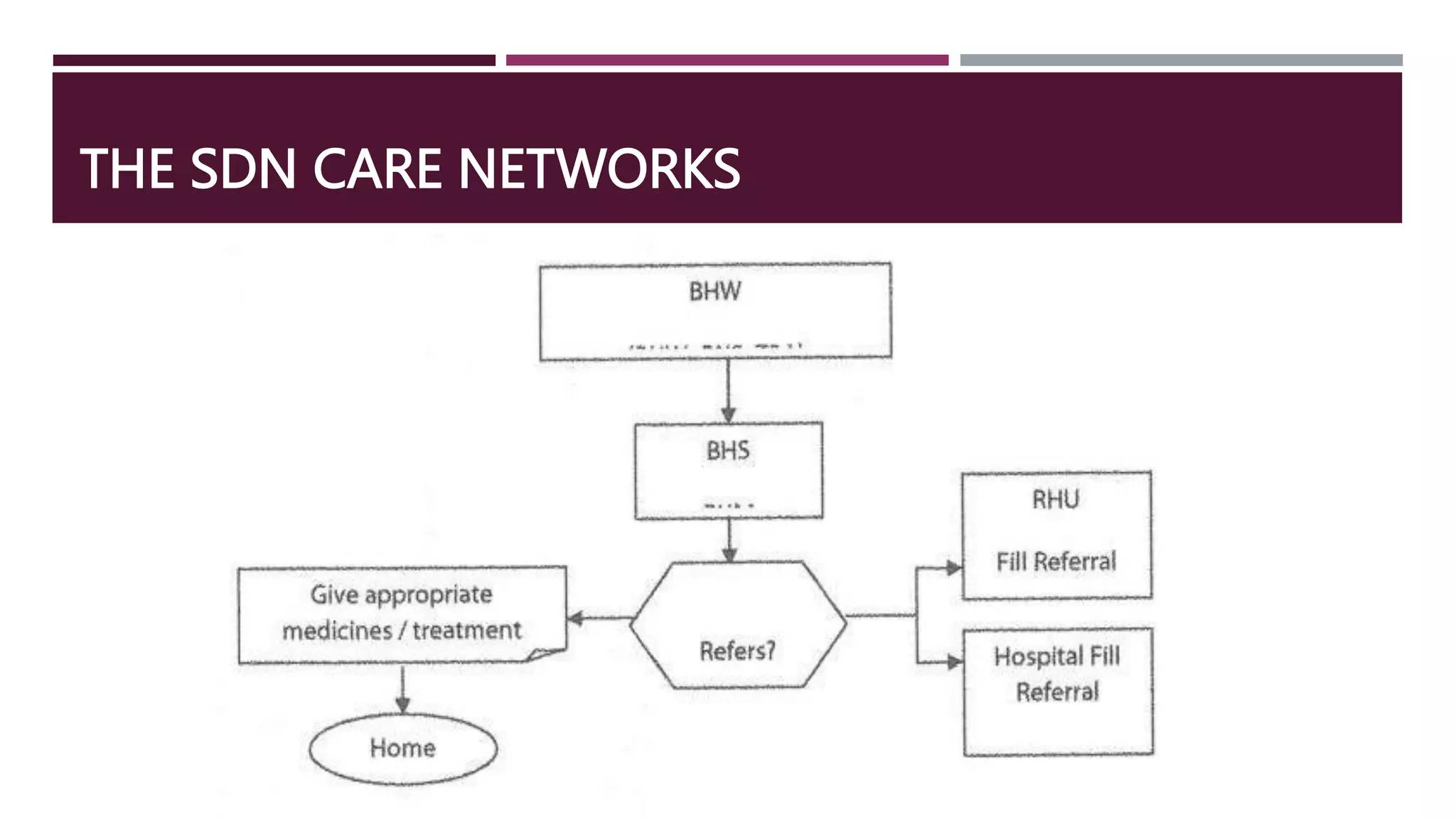
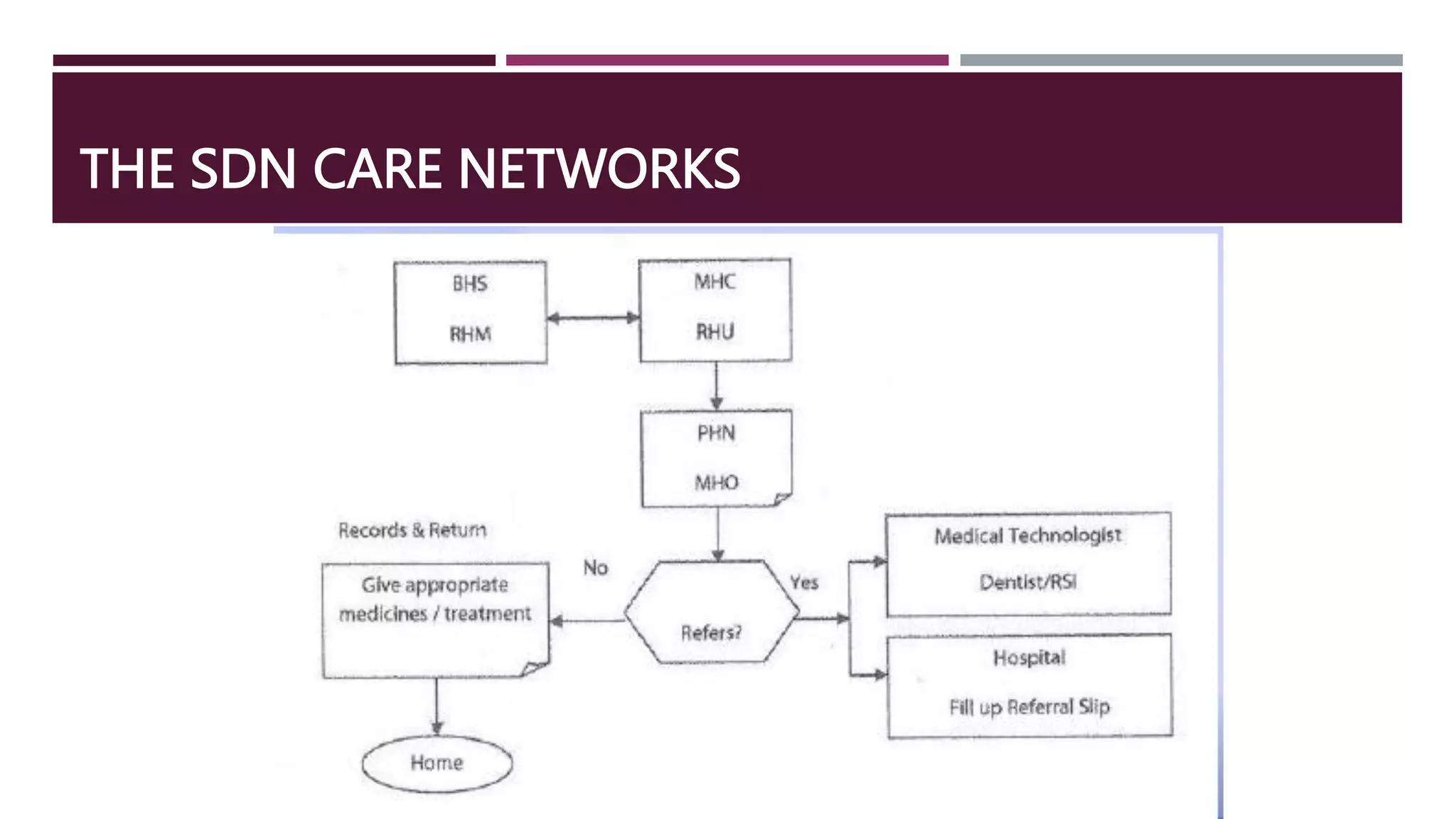
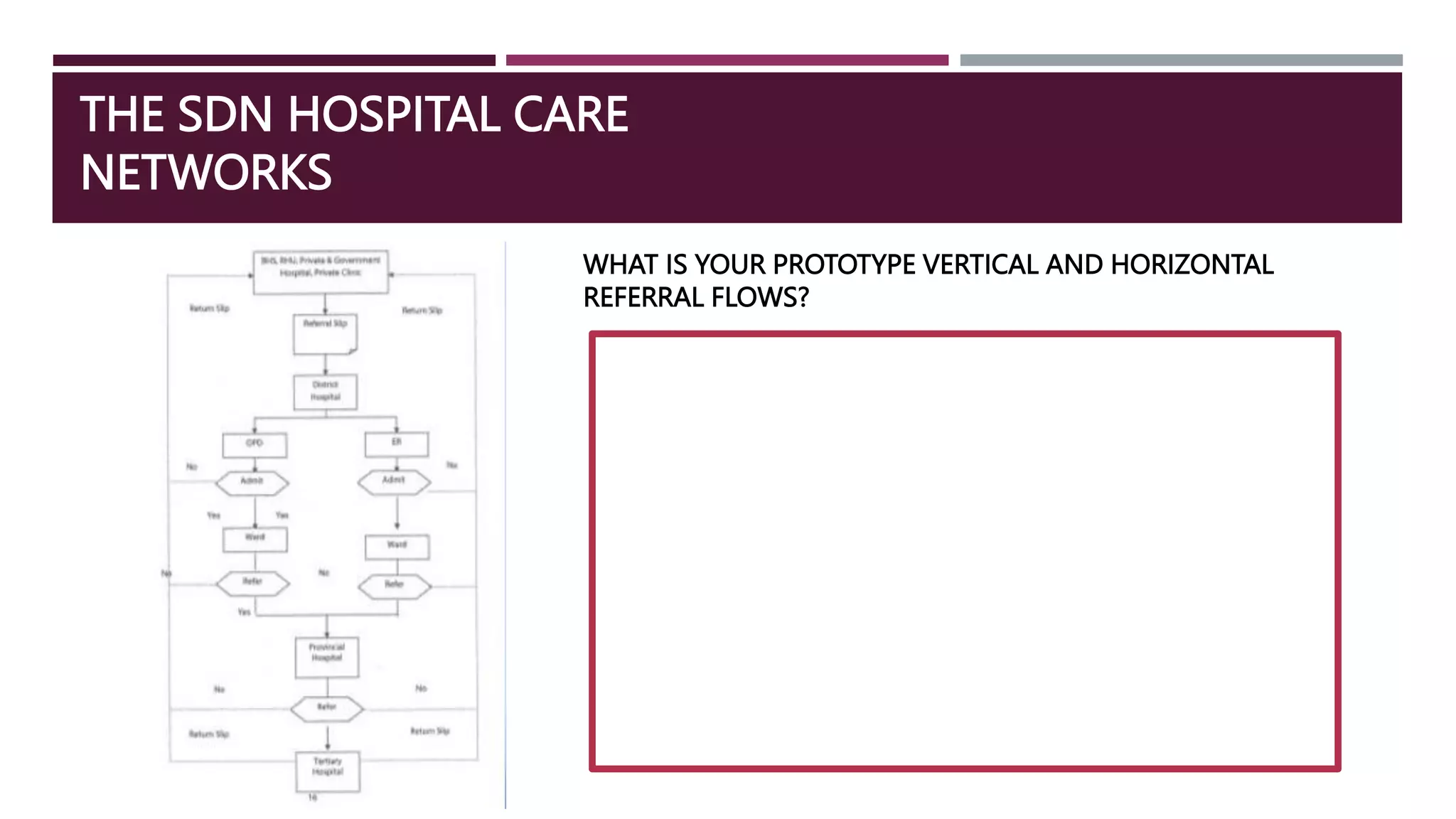
- SDNs are composed of primary, specialty and apex hospital networks to provide integrated care. Gaps remain in guidance for public-private integration and inter-facility referrals.
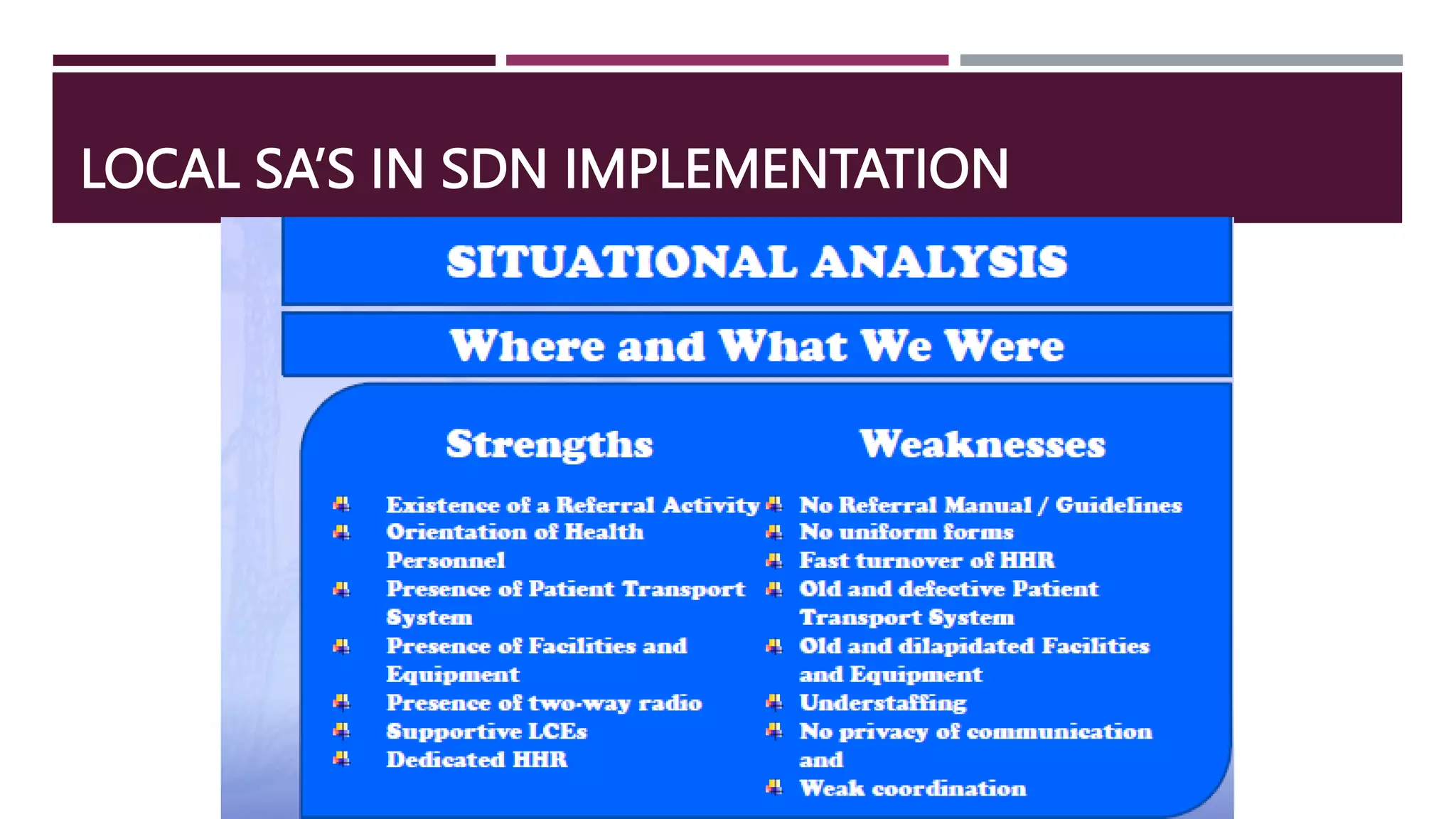
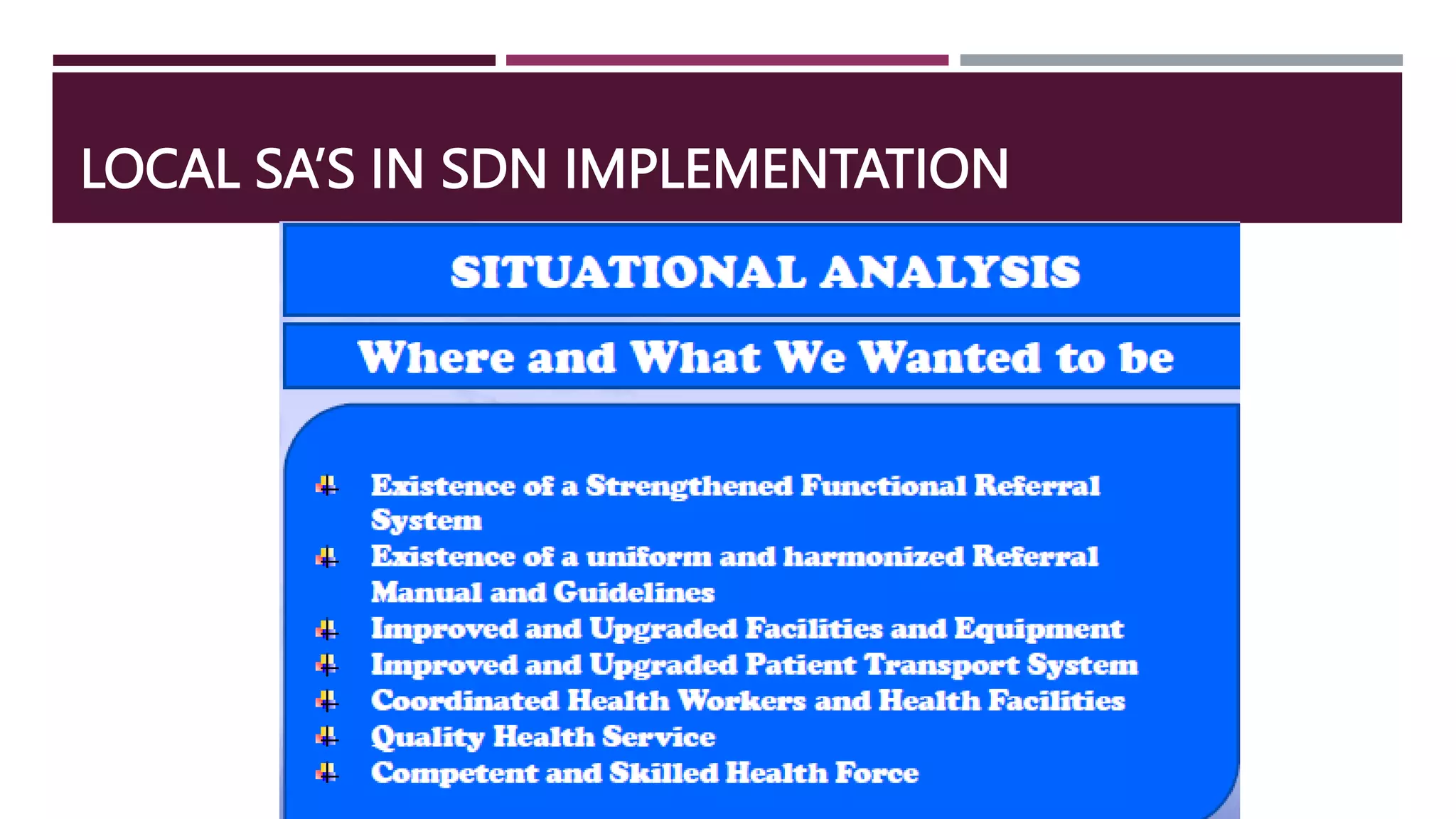
- Successful implementation requires addressing issues like governance, resources, incentives and sustainability at local levels. Perceived gaps include a